Abdominal aortic aneurysm treatment
Escrito por:In his first article, consultant vascular and general surgeon Professor Vassilis Hadjianastassiou explained what an abdominal aortic aneurysm is. But how are they treated? Professor Hadjianastassiou delves into the treatment options in this second article and provides important information to consider if having a procedure.

How is an AAA diagnosed?
An abdominal aortic aneurysm can be diagnosed with clinical examination of thin patients if the aneurysm size is greater than five centimetres in diameter. Therefore, the majority of cases are confirmed by an ultrasound scan of the abdomen, rather than clinical examination. The maximum diameter of the aorta (external to external wall) is the most important question answered during the scan. The surgeon will also examine your groins and behind the knees to look for other aneurysms in the femoral and popliteal arteries.
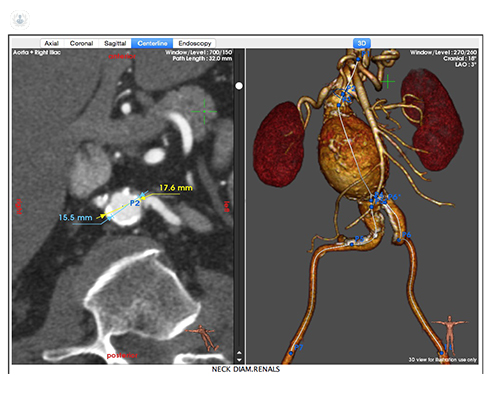
As soon as a surgeon requires more accurate information for either diagnosis or a repair plan, a CT-angiogram with intravenous contrast will be requested.

Will I need an operation?
It is possible that an AAA may, at some point, reach a size where surgery is indicated, typically when it exceeds 5.5 centimetres in men or 5 centimetres in women. A repair may be advised even before the normal repair threshold if the growth speed is fast. Due to surgery carrying significant risks, each individual patient’s health and reserves for recovery (particularly how well the heart, lungs, and kidneys work) must be taken into account before a decision to operate is made. Most patients will require some sort of tests on these organs and routine blood tests, including FBC, ESR, and electrolytes before operating.
What operation will be performed?
The traditional open surgery and minimally invasive endovascular aneurysm repair (EVAR) are the two options. Data suggests that for elective repair on large aneurysms (≥5.5 centimetres), EVAR is equally “good” in comparison to open repair in regard to overall survival. EVAR is less invasive, reduces AAA-related fatality and complications, and patients recover faster initially in the short-term. The caveat is life-long follow-up scans (normally a scan one and 12 months after the repair, and every five years if all goes well) to catch any leakage around the graft. Chances of further interventions being needed, such as repairing the leakage, are higher than that of open repair. Repair decision should be individualised per patient, considering the patient’s age, preferences, quality of life, sex, health reserves, and EVAR suitability (not everyone is suitable). The risks of surgery and consequent quality of life with either of the two options must be considered with careful counselling. Patients who are not suitable for traditional open surgery should be considered for EVAR.
Of all the AAA procedures performed, 10 to 25 per cent are open traditional surgery. The open procedure involves a vertical cut in the stomach and the diseased part of the aorta is replaced using a graft, which is an artificial tube. A graft designed like a pair of trousers will be used if the aneurysm extends into the iliac arteries. In some, it may even extend to the groins with separate cuts there. Death or heart attack are the main risks of surgery, which is around 1 in 20 patients overall. However, the risk of later complication after having a successful open operation is very low.
What is EVAR?
EVAR is a minimally invasive surgery, also known as “keyhole” type, where the abdominal aneurysm is repaired with a special stent. The aorta is strengthened by a fabric covered stent with wire support being fitted inside which prevents blood from flowing through the aneurysm. The idea is that if the blood does not flow through the weak aneurysm walls, the aneurysm should gradually shrink. The procedure can be performed under general or local anaesthesia involving access to the aorta via the groin area by small cuts. EVAR has a risk of death of about 2 in every 100, which is much lower than the traditional open surgery procedure. However, about 1 in 10 patients will require a subsequent smaller operation if a leak is detected around the stent during a follow-up. Heart attack and chest infection are general complications that may happen from an EVAR procedure; however, they are rare.
Further Information
Many people never experience problems from their AAA. Although, if the aneurysm does rupture, survival chances are small. For this reason, it is crucial to catch these aneurysms early, following them up if they are small and not causing symptoms, or having them repaired if a rupture seems more probable.
If you have recently been diagnosed with an abdominal aortic aneurysm or think you may be showing some symptoms, you can go to Professor Hadjianastassiou's profile and schedule a consultation.


