Areas of expertise – Ocular melanoma
Escrito por:Internationally esteemed consultant ophthalmologist Professor Bertil Damato speaks to Top Doctors in detail about ocular melanomas, rare but treatable cancers which occur within the eye and on the ocular surface.
Find out about diagnosis, treatment and prognosis in this comprehensive article about the condition by one of the UK’s leading practitioners of adult ocular oncology.

What is ocular melanoma?
Melanoma is a cancer of melanocytes, which are cells that produce light-absorbing melanin pigment. Normally, melanocytes stop reproducing themselves once there are enough of them in a tissue. When the genes that control such growth become dysfunctional, because of mutations, the melanocytes keep multiplying to form tumours (i.e., lumps) that invade surrounding tissues. When particular mutations develop, melanomas start to ‘metastasise’ through blood vessels or lymph channels to other parts of the body to form new tumours, known as ‘metastases’.
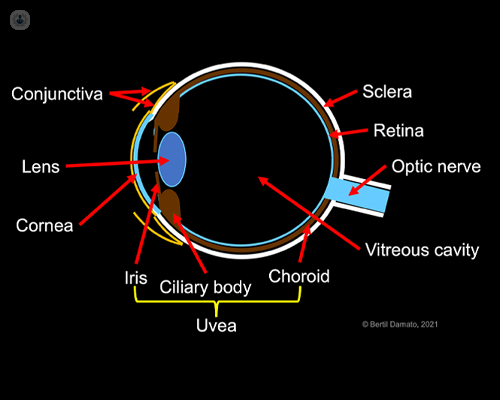
Almost all ocular melanomas occur inside the eye, in a pigmented tissue known as the ‘uvea’ (hence the term ‘uveal melanoma’). The large majority of these arise towards the back of the eye, in a cup-shaped part of the uvea known as the choroid, under the retina, which is the film of transparent tissue that provides sight. Some melanomas develop in the ciliary body, a ring of muscular tissue at the rim of the choroid, which adjusts the focus of the lens, so that we can clearly see objects both near and far. A few melanomas arise in the iris, the blue, grey or brown tissue that adjusts the size of the pupil to regulate the amount of light reaching the retina.
Rarely, ocular melanomas occur in the conjunctiva, which is a transparent membrane (‘skin’) that lines the outer surface of the eye and the inner surface of the eyelids.
What causes ocular melanoma?
Most uveal melanomas have no known cause. The chances of developing ocular melanoma are very low before adulthood, increasing with age and peaking at around sixty years. Men and women are affected in similar numbers. Ocular melanomas occur most commonly in fair-skinned individuals with blue eyes. Even so, they are rare, with uveal melanoma developing in only six individuals per million per year and conjunctival melanomas affecting only about one individual per ten million per year.
Some uveal melanomas arise from uveal naevi (called ‘moles’ in lay terms), which are benign tumours composed of melanocytes. Intraocular moles are found in more than one-in-twenty white adults with hardly any of these ever-showing malignant growth.
Rarely, uveal melanomas can arise from a ‘melanocytoma’, which is a small, black tumour that is usually located on the optic nerve at the back of the eye. Some develop from a congenital birthmark consisting of an over-population of melanocytes in the uvea (known as ‘congenital ocular melanocytosis’ or ‘Naevus of Ota’). Rarely, uveal melanomas occur in families with an inherited condition known as ‘BAP1 tumour predisposition syndrome’, which also causes cancer of the kidney, ‘pleural mesothelioma’ (a cancer of the lining of the lung), skin melanoma and other tumours.
Conjunctival melanomas can arise ‘de novo’ (i.e., ‘out of the blue’) or from benign moles or from ‘primary acquired melanosis (PAM)’ (i.e., overgrowth of melanocytes forming a brown conjunctival patch developing after birth with no obvious systemic disease).
Can ocular melanomas be prevented?
Some melanomas of the iris and conjunctiva develop after prolonged exposure to the sun, as can other cancers, such as carcinoma of the conjunctiva and eyelids. It is advisable to visit an optometrist or ophthalmologist every 1 to 2 years so that melanoma and other conditions, such as glaucoma and cataracts, can be detected and treated as early as possible.
Symptoms of ocular melanoma
Many uveal melanomas are totally asymptomatic when they are detected on routine eye examination by an optometrist or ophthalmologist if the patient has presented for other reasons (e.g., broken spectacles, two-yearly check-up, glaucoma, cataract). Choroidal melanomas tend to damage the retina to cause blurred or distorted vision or flashes of light. Ciliary body melanomas can damage the lens to cause cataract. Most iris melanomas are visible to the naked eye so that they are noticed by patients, relatives or friends; some block the normal flow of fluid from the eye to cause a high intraocular pressure (i.e., glaucoma). Without timely treatment, uveal melanomas can make the eye blind, inflamed and painful.
Conjunctival melanomas may develop as a flat, brown patch on the ocular surface, known as ‘primary acquired melanosis (PAM) with atypia’, or they can form a nodule, which can be black, grey, brown, pink, or red.
How are ocular melanomas diagnosed?
Diagnosis of uveal melanomas is based on ocular examination with a slit-lamp (i.e., microscope) and ophthalmoscope, aided by a variety of investigations, which include colour photography, autofluorescence imaging, optical coherence tomography and ultrasonography. In some cases, the diagnosis needs to be confirmed by biopsy, obtaining a tumour sample with a type of needle by means of an operation.
Most nodular conjunctival melanomas are diagnosed by their size and appearance, with some requiring removal for laboratory investigation. Primary acquired melanosis (PAM) may need biopsy to determine whether the melanocytes are benign or malignant.
When differentiation between ocular melanoma and naevus (mole) is not possible, the tumour is kept under long-term review, repeating examinations every four to 24 months according to the estimated likelihood of malignancy.
Investigations are also performed to detect any tumours in other parts of the body.
Treatments for ocular melanoma
The main objectives of treatment are to protect life and, if possible, to conserve the eye with useful vision.
Before starting any treatment, the risks and benefits of every therapeutic option, the chances of conserving vision and the eye and the survival probability are carefully explained so that the most suitable form of treatment is selected according to each individual patient’s needs and priorities.
Uveal melanoma
- Plaque brachytherapy
The first choice of treatment for choroidal melanoma is radiotherapy delivered with a disc-shaped radioactive ‘plaque’, which is sutured to the wall of the eye (i.e., the sclera) directly over the tumour and removed three to five days later once the entire tumour has received enough radiation to prevent further growth. Plaque insertion and removal are performed under local anaesthesia with sedation in an operating theatre, with inpatient hospital care while the radioactive plaque is in place.
- Proton beam radiotherapy
If plaque radiotherapy is not possible, because of the size, shape or location of the uveal melanoma, my next choice of treatment is proton beam radiotherapy. First, four tiny tantalum (non-magnetic metal) buttons known as ‘markers’ are sutured to the sclera so that the tumour can be localised for treatment, by taking X-rays of the eye. This is done under local anaesthesia with sedation in an operating theatre as a day case. A few weeks later, a 3-D computerised model of the eye is generated so that plans can be prepared to aim the proton beam at the tumour, if possible, avoiding the optic nerve and lens. This takes one to two hours and is done as an outpatient at Clatterbridge Cancer Centre, on the Wirral Peninsula. One or two weeks after that, the radiotherapy is administered over four consecutive days at Clatterbridge Cancer Centre, with each treatment session lasting one to two hours. This is done with the patient sitting on a special chair, looking at a strategically located light, and with the head kept still by means of a face mask.
- Laser therapy
With ‘transpupillary thermotherapy (TTT)’, each part of the tumour is gently heated for about a minute to cause tumour cell death. With ‘photodynamic therapy (PDT)’, the laser activates a drug that accumulates in the tumour after it is injected into the arm or the eye. Laser treatment needs to be administered over several sessions. It is not as reliable as radiotherapy so that it is reserved for very small choroidal tumours. In some patients, laser treatment can reduce fluid leakage from a tumour after radiotherapy, improving vision.
- Surgical excision
Rarely, the tumour can be removed surgically, either intact, through a ‘trapdoor’ in the wall of the eye (i.e., ‘exoresection’) or by aspirating the tumour through a fine tube (i.e., ‘endoresection’).
- Enucleation
If it is not possible to conserve a comfortable and useful eye, it may be necessary to remove (i.e., ‘enucleate’) the eye and to fit a cosmetic prosthesis (‘artificial eye’). My colleagues and I have studied quality-of-life studies in more than 1,500 patients, and we have found that wellbeing after enucleation is similar to that after radiotherapy.
Conjunctival melanoma
- Chemotherapy
Mitomycin-C drops are used to treat primary acquired melanosis (PAM) if biopsy indicates that there is a significant risk of invasive melanoma developing.
- Surgical resection
Nodular (i.e., lumpy) conjunctival melanomas are surgically removed, under local anaesthesia in an operating theatre as a day case.
- Radiotherapy
If laboratory examination shows deep invasion of a nodular melanoma, radiotherapy is delivered either with a radioactive plaque, which is left in place for about one day, or with a (strontium) radioactive applicator, which is held over the treated area for a few minutes every day for four or five days, or, rarely, with a proton beam. The radiotherapy is administered about one month after surgical resection, once the wound has healed.
- Long-term surveillance
After treatment, the eye is examined at increasing time intervals to ensure that the tumour responds to the treatment and to detect and treat any tumour re-growth and side effects. For example, laser treatment or injections into the eye may be required if the vision is affected by fluid leaking from the irradiated tumour. Liver scans and other investigations are performed regularly if there is a risk of tumours developing in other parts of the body.
Prognosis of ocular melanoma
Uveal melanoma
The chances of conserving the eye and useful vision depend on the size and location of the tumour with respect to optic nerve and macula.
Metastatic disease develops almost exclusively in patients whose tumour shows particular genetic abnormalities, such as chromosome 3 loss, chromosome 8 gain, and mutation of the BAP1 gene. With these aberrations, the survival prognosis is worse in patients with a large tumour and/or an epithelioid (i.e., ‘round’) cell shape.
The risk of metastasis is estimated by determining the tumour size and extent and by performing laboratory tests on a tumour sample, which is obtained by biopsy.
Conjunctival melanoma
The chances of conserving vision and preventing metastatic spread depend on the tumour size, location and extent. Unlike uveal melanomas, conjunctival tumours can spread to glands in the neck.
Patients are referred to a medical oncologist for long-term surveillance aimed at detecting and treating any tumours in other parts of the body.
If you’re concerned about ocular melanoma or related eye conditions, visit Professor Damato’s Top Doctors profile, here, to book an appointment.



