Cracked backs and kyphoplasty: an expert’s guide to vertebral compression fractures
Escrito por:Back injuries can be very serious. Your spine is not just part of your skeleton – it also contains important nerves that help to control your body. One type of injury that can occur is a vertebral compression fracture. Top neurosurgeon Mr David Bell explains.

What are vertebral compression fractures?
When the block-like part of the vertebra (spine) responsible for bearing weight is squashed or compressed, these bones can fracture. This occurs most commonly in the lumbar (lower spine) but can happen anywhere in the spine. This injury is called a vertebral compression fracture.
How do we get vertebral compression fractures?
Vertebral compression fractures may be caused by one or more of the following factors:
- Osteoporosis – a bone disease that causes a loss of bone density. This weakens the bones, increasing the chance of fracture. Osteoporosis can affect anyone, but is particularly common in post-menopausal women.
- Pathological – other diseases, such as metastatic cancer, osteomyelitis (bone infection) and Paget’s disease can increase the chance of fractures.
- Trauma – it takes a lot of force to cause a vertebral compression fracture, which could be the result of a severe fall or car accident. However, if the patient is afflicted with osteoporosis or another condition that weakens the bones, less force is needed to cause a fracture.
How do you know if you have a vertebral compression fracture?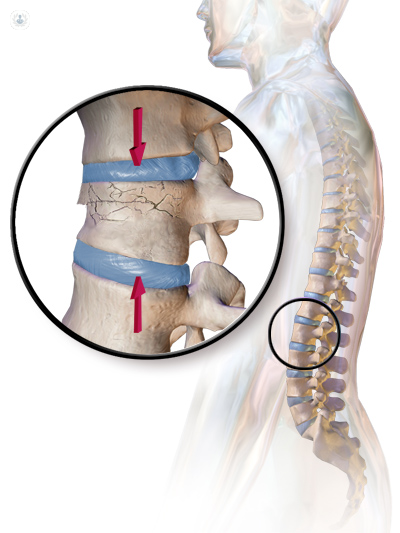
Symptoms of a vertebral compression fracture to watch out for include:
- Back pain – particularly in the lower back.
- Numbness or tingling – if the nerves in the spine become compressed by the fracture it can have these effects.
- Incontinence or urinary retention – this can be caused by fragments of bone from the fracture pressing on the spinal cord.
Diagnosis of vertebral compression fractures can be made using imaging techniques such as X-rays, MRI or CT scans.
How are vertebral compression fractures treated?
Possible treatments for vertebral compression fractures include:
- Back brace
- Resting and applying ice
- Pain medication, such as NSAIDs (non-steroidal anti-inflammatory drugs) and muscle relaxants
- Exercise – follow your doctor’s instructions as to when you are ready to engage in physical activity again and which exercises to do in order to rehabilitate the muscles in your back and prevent further osteoporosis.
There are also surgical options if the conservative treatments listed above are ineffective or if the fracture is causing neural problems.
Kyphoplasty
A minimally invasive option, kyphoplasty involves inserting a narrow tube into the spine via a keyhole incision in the back. The surgeon can monitor the position of the tube with X-ray images and guide it to the damaged vertebral body. There, a special balloon is passed through the tube to the vertebra and inflated, where it creates a space inside the bone and may also partially restore it to its natural height. The balloon is then removed and a cement-like material (polymethylmethacrylate) is injected to fill the void, quickly hardening to stabilise the bone. The desired result is to stop the micro-movements of the fractured vertebra which cause the pain.
Vertebroplasty
A vertebroplasty is very similar to a kyphoplasty – image guidance such as fluoroscopy is used to position the tube and the cement-like mixture is injected into the space. The difference is that a balloon isn’t used to create the space in the vertebra first.
How to prevent vertebral compression fractures?
Osteoporosis is a major factor in causing vertebral compression fractures, and you can reduce your risk of osteoporosis (and therefore reduce your risk of vertebral compression fractures) by taking the following measures:
- A healthy, balanced diet, rich in calcium and vitamin D, which strengthen the bones
- Exercise – especially weight-bearing exercise, which promotes bone strength
- Stop smoking


