Uncovering the causes of migraine
Autore:Migraine is more prevalent than diabetes, epilepsy, and asthma combined. It causes 25 million lost days of work or school every year in the UK. For a long time, our understanding of the causes of a migraine was limited. In recent years, however, we’ve seen significant advances in theories about how migraines occur. In this article, we speak to Dr Stefan Schumacher, a consultant neurologist based in Greater Manchester with a special interest in the treatment of a headache and migraine.
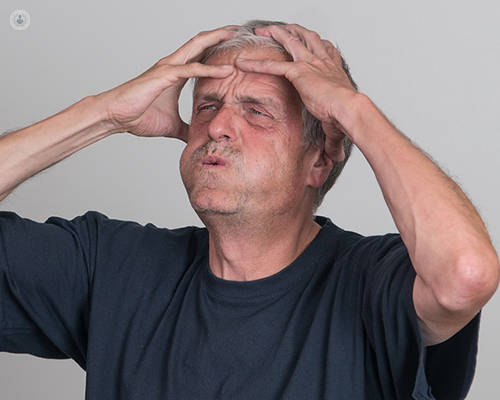
What does a migraine feel like?
My patients often describe to me that they have a pressure above their eyes on the whole front head, which then worsens into a throbbing pain or a pulsing sensation. This can either be on one side of the head or on both sides. It can also spread to the rest of the head. This pain can build up quite quickly in hours or sometimes even minutes. The pain is significant and horrible for the patients. The migraine itself can go alongside a very high sensitivity to light, sounds, smells and touch. Patients can sometimes not stand the smell of food and perfume. Many migraine patients have to lie down and find relief in a dark room. A high number of our patients feel sick with the pain and some also vomit often quite frequently. However, there are quite a number of my patients who just experience nausea and no vomiting. The actual migraine attacks are often also described as lightheadedness and slight dizziness. Afterwards patients feel weak, sometimes even confused – and of course, often suffer from low mood. We distinguish two “warning signs” for migraine: One is called prodrome and the other one is aura.
Prodrome
These start one or two days before a migraine. The symptoms are:
- mood changes
- depression
- neck pain
- increased thirst and urination
- some patients also yawn more frequently
These so-called prodromes occur less than auras, which is the second pre-stage and warning of a migraine.
Auras
These normally affect the visual system and show with flashing lights or zig-zag vision. Some patients also have visual loss. These auras build up gradually and can last between 20 and 60 minutes. Sometimes auras can be caused by certain movements or speech disturbances. Auras can also be triggered by a foul smell or tobacco. The patient can also have sensory symptoms (pins and needles) in the arm or legs. Sometimes I see weakness or numbness in the face or one side of the body. Aura can even affect the speech so that patients cannot express themselves. In rare cases, patients have unusual jerky movements. In my clinical experience, many of my patients have a migraine without an aura and this has been shown in large international studies.
Why do I get a migraine?
There is not one cause for migraine. Migraine is a complex condition. We used to think that a migraine was caused by problems in the cerebral arteries with blood flow. However, today’s understanding is that chemical compounds and hormones also play a very important part, for instance, serotonin and oestrogen. These so-called trigger chemicals cause a narrowing of the blood vessels and this is the theory behind how a migraine happens. There is a lot of research currently being done in this area to further our understanding of how these factors interact.
What triggers a migraine?
Although an actual cause for a migraine as such is also not yet identified, in my long year work with migraine patients, I have often seen certain triggers which worsen headaches. These are:
- stress in any form
- depression
- sleep deprivation
- hormonal shifts
- tiredness
- insomnia
Certain foods and drinks can sometimes worsen or sometimes even cause a migraine, especially:
- red wine
- cheese
- chocolate
- nuts
(Unfortunately, these foods and drinks are often very well-liked by patients and they all enjoy them!)
I also see patients whose migraines are brought on by changes in the weather. Finally, a lot of migraine patients are light sensitive and hence flickering lights in certain clubs or even from PC screens can cause or worsen a migraine
.
Why are some people more prone to a migraine than others?
In general, more females suffer from migraines than males. I assume that the reason for this is that the hormonal changes in women. The fluctuation in oestrogen seems to trigger the headaches. For example, many of my female patients suffer from increased migraine before or during their periods. I call this menstrual migraine. Meanwhile, it is always very interesting for me to see that women who become pregnant or enter the menopause often have much fewer headaches. Certain contraceptives like combined oral hormones worsen the migraine. It is therefore very important for us to ask female patients if they are on contraception and, if so, what medication they are taking. Many of our patients have a family history of migraines, and therefore have a high increased risk for developing migraines. I sometimes have patients who have migraines through three or even four generations. Finally, a patient’s age plays a very significant part in migraines. They start normally in adolescence and are less severe in ages 50-70. Migraine is not a very frequent disease we find with elderly patients.


