Abdominal Aortic Aneurysm – AAA
Written by:There are different kinds of aneurysms, as they can happen in any artery in the body. Abdominal aortic aneurysms are the most common ones. In this article, consultant vascular and general surgeon Professor Vassilis Hadjianastassiou details what they are and what patients should know.

What is an aneurysm?
An aneurysm happens when the walls of the arteries weaken. The arteries are what make up the pipework that carries the blood around the body. The pressure of the flow of blood then makes the walls stretch and balloon out to form an “aneurysm”, which essentially means a weakened arterial wall segment which can burst.
Even though aneurysms can happen in any artery of the body, the most common location is in the aorta. This is the main artery in the abdomen; this is called an abdominal aortic aneurysm (AAA).
In order to have an idea where the location of the aorta is, imagine the artery running from the heart, down through the chest, and then into the tummy. Around the location of the belly button (top of the hip level in overweight patients), the artery then divides into two known as the iliac arteries. These deliver blood to organs in the pelvis and legs. The iliac arteries can also form aneurysms, which frequently co-exist simultaneously with abdominal aortic aneurysms.
Aneurysms grow larger with time and do not just appear suddenly; they usually develop over several years. Therefore, smaller aneurysms, which are not likely to rupture, can be followed-up with routine scanning and clinical examination. However, depending on the location of the aneurysm, when it reaches a certain size the risk of it rupturing becomes too great to just sit and watch. If an aortic aneurysm bursts this would result in massive internal bleeding, which is fatal for about 90 in every 100 people. Your doctor may advise to have the aneurysm surgically “repaired” once it reaches a certain width size.
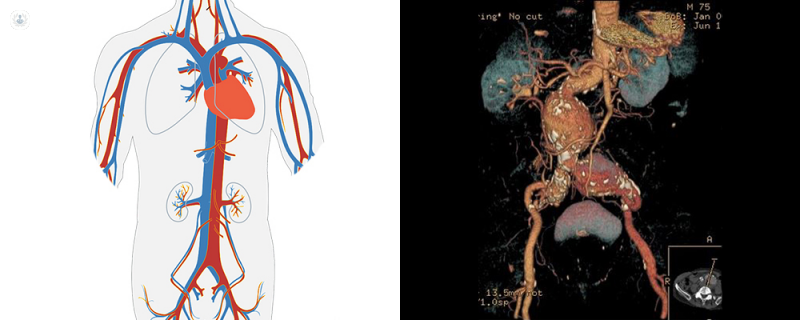
Right: Imaging of an abdominal aortic aneurysm, seen centre, in a real patient of Prof. Hadjianastassiou.
What is an abdominal aortic aneurysm – AAA?
A normal aorta is approximately 1.5 to 2 centimetres in width, which is about the size of a garden hose pipe. An abdominal aortic aneurysm is officially diagnosed if any part of the aorta within the abdomen is 3 centimetres or more in diameter. If it is more than 2 centimetres but less than 3, it is a not-so-concerning “ectasia” (not aneurysm).
Aneurysms are typically found by chance while having a physical examination or scan for something else. Unless they have burst or blood has clotted inside them or, sometimes, they are pressing on a nearby structure and this alerts the patient, they don’t usually cause symptoms.
As an aneurysm grows, it can get so large where there is then a significant chance of the artery wall bursting and bleeding. This is known as a “ruptured aneurysm”, which is a serious and life-threatening emergency.
Why do we get aneurysms?
Though they can affect anybody, aneurysms are more common in men, patients suffering with hypertension (high blood pressure), patients who smoke, and in patients over the age of 65. Among UK men invited for screening at their 65th birthday, about 1.5 per cent of them have an abdominal aortic aneurysm (> 2.9 centimetres in diameter). It is thought that around one to three in every 100 men over 65 years old will develop an aneurysm, however, not all aneurysms will be of a significant size. As well, around one in 100 will have an aneurysm large enough to require surgery. Despite being six times rarer in women, aneurysms are more likely to rupture once they are present.
The risk of developing an aneurysm seems to be partially hereditary, depending on the patient’s genes. Male relatives who are close to an affected patient are more likely to get an aneurysm themselves. However, most patients’ family history has no known aneurysms, so genes are not wholly to be blamed for this! High blood pressure and smoking are known to increase the risk and the size of the aneurysm once they are present.
Abdominal aortic aneurysms vary in size. On the whole, once an AAA has developed, it usually gets gradually larger. Although, the speed at which it grows varies from patient to patient. An AAA growth may be slowed down by taking certain medication (e.g. statins, ACE-inhibitors, beta blockers, etc) if it is suitable for the patient and the doctor has advised it.
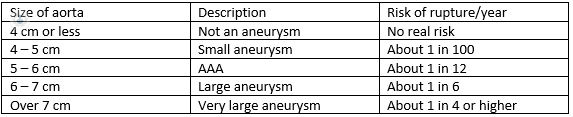
The risk of the aneurysm rupturing at each diameter size can be broadly summarised in the table below:
Annual screening intervals for 3 to 4.4 centimetre and 3-month interval screening for 4.5 to 5.4 centimetre aneurysms are recommended by the UK National Health Service.
If you are having doubts or concerns about having an abdominal aortic aneurysm, or would like further information, you can schedule a consultation on Professor Hadjianastassiou's profile.