An introduction to macular oedema
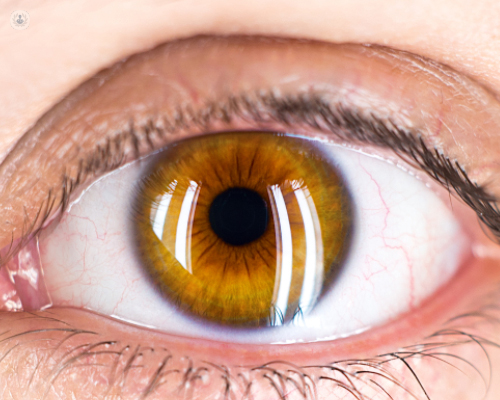
Written by:Macular oedema is an eye condition which causes poor quality vision. The macula is found near to the central part of the retina and its function is to provide clear images when you look ahead. Patients with macular oedema will complain of distorted and blurred vision, which is caused by a build-up of fluid. In this article, Dr Rupal Morjaria, highly experienced consultant ophthalmologist, gives us an introduction to the condition, what symptoms we should look out for and what patients can expect from treatment.
What causes macular oedema to occur?
Macular oedema has a number of causes but is commonly linked to diabetes. It can also be caused by a lack of oxygen supply to the eye or as a consequence of eye surgery, which may cause oedema or swelling to the central macular region. This leads to blurry central vision and a distortion of lines. Ageing may cause macular oedema, known as age-related macular degeneration, as may some rare genetic disorders.
What are the main symptoms?
The main symptoms of macular oedema are:
- decreased vision
- difficulty when reading
- distortion when looking at straight lines
You should consult your ophthalmologist if you have noticed changes in your vision, particularly in your central vision.
What is the most effective treatment for macular oedema?
Effective treatment of macular oedema depends on the cause, the location and the quantity of the oedema in the eye. Patients may benefit from laser treatment to reduce the oedema if it is found to be off the central fixation point of the eye. If it is central, however, Anti VEGF injections, used to prevent loss of vision, may be used to better effect.
Is it hereditary or can surgical procedures be a life-long fix to the problem?
Although conditions like diabetes are hereditary, currently macula oedema isn’t thought to be. If macular oedema is secondary to a rarer genetic condition such as retinitis pigmentosa, then it may be hereditary.
Although there is no cure for macular oedema, early diagnosis and consistent follow ups with a specialist ophthalmologist will allow patients to manage the condition and to enjoy a good level of vision. Regular check-ups to monitor the quality of the patient’s vision are important and treatments may be repeated if symptoms redevelop as time goes on.
What would your advice be to anyone suffering from this condition?
If you are suffering from macular oedema you should take care to monitor your vision yourself but also keep up with regular appointments with your ophthalmologist. Your specialist will need to do regular scans to follow the progression of your condition, which may perhaps lead to further treatment.
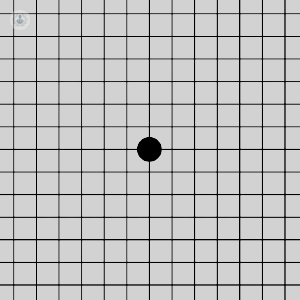
To monitor your vision at home, you can use the Amsler chart. To assess your central vision, you should look at the chart with one eye at a time and check for distortion in how you perceive the lines.
You can ask your GP to check your blood pressure, blood sugar and cholesterol to monitor your general health. Additionally, you should keep up a healthy lifestyle by eating a balanced diet, taking regular exercise and getting enough sleep. Keeping well will help to minimise risk factors associated with the development of the condition.
If you are concerned about your eyesight or think you may be suffering from macular oedema, you can visit Dr Morjaria’s Top Doctors profile to book a consultation with her.


