Ask an expert: How is anterior uveitis treated?
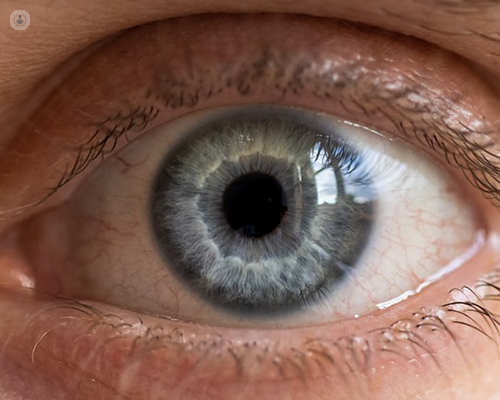
Written by:Anterior uveitis, also known as iritis, occurs when the iris, the coloured part of the eye, becomes inflamed. This can cause increased sensitivity to light and a sharp ache in the eye area. If left untreated, patients with anterior uveitis can develop serious complications such as cataracts and glaucoma, so seeking out treatment promptly is essential. In this informative article, leading consultant ophthalmic surgeon Mr Harry Petrushkin expertly outlines the causes and symptoms of the condition, as well as explaining what patients can expect from treatment and recovery.
What causes anterior uveitis?
In more than three quarters of patients, no exact cause is found. In some cases, patients suffering from other inflammatory conditions, such as inflammatory bowel disease or arthritis, can also develop anterior uveitis.
What are the symptoms of anterior uveitis?
Anterior uveitis can affect just one or both eyes. The most commonly experienced symptoms are:
- redness in the eye
- pain in the eye, which can worsen while focusing the eye or when in brightly lit areas
- sensitivity to light
These symptoms can develop gradually over time or more rapidly and are usually acute (of short duration). A small minority of patients will experience chronic anterior uveitis, which can in some cases be painless. This can affect the eye’s internal structure and requires treatment despite not being painful.
How is anterior uveitis treated?
Anterior uveitis is usually treated by a combination of eye drops which work together to heal the eye. These include:
- steroid eye drops, to reduce inflammation in the iris
- dilating eye drops, to relieve pain and allow the eye to rest
- drops which reduce the pressure within the eye, which may be elevated by the steroid treatment, or by the inflammation itself
After just a few days of taking the drops, the symptoms of the condition are usually resolved but it is necessary to complete the treatment to ensure that the inflammation has fully cleared. If the treatment is ineffective in treating the symptoms, it is important to see a specialist promptly.
Episodes of anterior uveitis can vary in their duration but the course of treatment usually lasts from six to eight weeks. Side effects can occur from extended use of steroid drops so they are only prescribed for as long as is necessary. Patients suffering from chronic episodes of anterior uveitis, or other conditions may also need to undergo blood tests or X-rays to fully investigate the problem and to ensure that the right treatment is prescribed.
If you are concerned about your eye health or by symptoms of anterior uveitis, you can book a consultation with Mr Petrushkin by visiting his Top Doctors profile.


