Causes and diagnosis of the most common types of jaundice
Written by:Jaundice is characteristically known for its yellow effect on the skin, but unbeknownst to many, there are different types as well as different causes. Professor Roger Williams CBE explains the symptoms, causes and diagnosis of the most common types of jaundice.
What are the symptoms of jaundice and how do I know I have it?
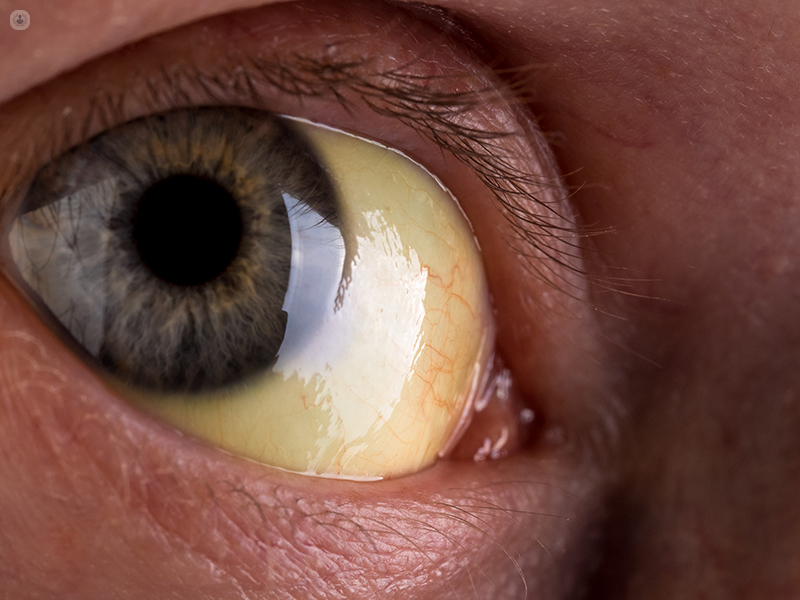
A patient will know he/she has jaundice when in addition to having yellow eyeballs, they also have dark urine and pale stools. The most important decision when choosing treatment is to diagnose which category of jaundice the patient has.
Two common categories are obstructive jaundice and parenchymal jaundice. While obstructive jaundice requires surgical relief, parenchymal may only need medical treatment.
What causes obstructive jaundice?
The most common cause of obstructive jaundice occurs in the gallbladder. During the passage of a gallstone from the gallbladder to the bile duct, rather than passing through completely, the gallstone becomes lodged and obstructs the bile flow. To remove the gallstone from the gallbladder, surgical treatment is required.
The second most common cause is pancreatic cancer. In this case, the obstruction occurs in the lower end of the common bile duct.
How is obstructive jaundice diagnosed?
The patient will need to be referred to a Consultant Hepatobiliary Surgeon who will likely carry out further investigations to discover the exact cause. This can be in the form of:
- An ultrasound examination
- An ERCP (Endoscopic retrograde cholangio-pancreatography)
- A MRCP (Magnetic resonance cholangiopancreatography) examination to define the site of the obstruction
Characteristic findings in liver blood tests of a patient with obstructive jaundice are:
- High alkaline phosphatase, a type of enzyme which if high, can indicate that there is a problem with your liver.
- Raised bilirubin levels (a slightly yellow substance in your blood)
Often the patient experiences itching as the jaundice worsens, sometimes manifested by an episode of cholangitis or other symptoms which include shivers, rigors and high temperatures. Cholangitis occurs when there is obstruction to bile flow and a secondary bacterial infection.
What causes parenchymal jaundice?
Parenchymal jaundice is caused by a viral hepatitis, usually hepatitis A or B. If the patient is from overseas, hepatitis E could be a potential cause.
The patient may have general symptoms of feeling unwell, particularly a poor appetite and nausea.
Hepatitis C is rarely acute, meaning it begins gradually and is treatable with the new antiviral agents available. Patients with an acute viral hepatitis usually require supportive therapy only. Furthermore, it is important that the patient’s nutrition is maintained despite a lack of appetite.
In parenchymal (hepatic) jaundice, the cause is a disease of the liver itself, such as
- Infective hepatitis, also known as viral hepatitis (inflammation of the liver)
- Drug toxicity (when the liver is poisoned)
- Cirrhosis (when liver tissue becomes scarred)
How is parenchymal jaundice diagnosed?
A more chronic liver disease such as autoimmune hepatitis, where drug treatment with Prednisolone is particularly effective, will require further investigations into serum autoantibodies levels and liver biopsy.
Often, a CT examination will be carried out to show any characteristic changes in cirrhosis, a scarring of the liver.
Patients with possible chronic liver disease as well as those with acute viral hepatitis who do not begin to improve after a few days need to be referred to a consultant hepatologist.
Acute Liver Failure (Fulminant Hepatitis)
A rare but very important diagnosis to make is that of acute liver failure. One particular cause of acute liver failure which must be considered urgently is a paracetamol overdose; the earlier the antidote is given, the better the chances of halting the progression of the liver injury.
Haemolytic jaundice
A third category of jaundice is haemolytic jaundice. In this case, it develops in association with an increased breakdown of red blood cells. Haemoglobin is a protein found in red blood cells which carries oxygen and in haemolytic jaundice, blood tests show a falling haemoglobin level and a rising jaundice level.
Professor Roger Williams CBE is a highly esteemed Hepatologist in London. Visit his profile for more expertise on hepatology and to book an appointment.


