Diagnosing prostate cancer: Nuclear Magnetic Resonance and biopsy
Written by:Nuclear Magnetic Resonance (NMR) and Biopsy provide urologists and oncologists with information for the diagnosis and prevention of prostate cancer.
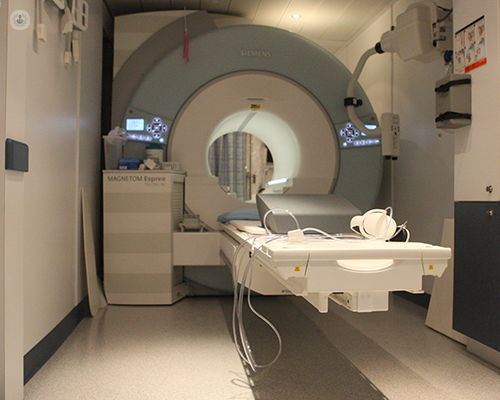
Multi-parameter Nuclear Magnetic Resonance in prostate cancer diagnosis
Although nuclear magnetic resonance has been used in the diagnosis of prostate cancer since the 1980s, its usefulness has increased in recent years by combining conventional imaging of T1 and T2 (morphological) with various functional imaging modes such as diffusion DWI), dynamic contrast study (DCEI) and spectroscopy (MRSI). This is known as multi-parameter Nuclear Magnetic Resonance. Multi-parameter NMR is the imaging technique with greater sensitivity and specificity in prostate cancer diagnosis, offering information for, the location and the extent of the tumour. Multi-parameter NMR is also useful to detect tumours of the anterior area of the prostate that are not reached with a conventional biopsy.
Types of Multiparametric Magnetic Resonance Imaging (mpMRI)
Morphological MRI, with images in T1 and T2: T2 images show the zonal anatomy of the prostate. The central area consists of a nodular zone and the signal intensity depends on the amount of glandular tissue that is hyperintense (clear) and the amount of stromal tissue that is hypointense (dark). The normal peripheral area of the prostate looks hyperintense because it has many secretions ducts. Prostate cancers that occur in 70% of cases in the peripheral area are seen as a hypointense (dark) lesion surrounded by an area of normal tissue that is hyperintense (clear). In contrast, cancers of the central area of the prostate that is normally hypointense are very difficult to differentiate in T2 images.
Benign prostatic lesions such as benign prostatic hyperplasia, prostatitis, bleeding, or post-treatment with radiation therapy or with hormones are also seen as hypointense, making it difficult to differentiate them from cancer. Therefore, the sensitivity and specificity of morphological MRI (T1 and T2) are very variable in the diagnosis of prostate cancer. The main indications of T1 and T2 imaging for prostate cancer are the assessment of capsule and seminal vesicle invasion.
Functional NMR: This is a dynamic study with contrast imaging and spectroscopy to increase the sensitivity and specificity of MRI in the diagnosis of prostate cancer according to the different phenotypes of the tumour. Cellular density is assessed with diffusion weighted imaging (DWI), angiogenesis, which is the production of blood vessels, is assessed with dynamic contrast study (DEC) and tumour metabolism is assessed with spectroscopy.
Diffusion Weighted Imaging (DWI): DWI reports on the movement of water molecules. Protons are more mobile in normal prostate tissue, while their movement is restricted in areas with higher cell density such as tumour sites. Therefore, prostate cancer in both the peripheral and central areas has a much lower diffusion than in areas of benign tissue. 22 studies observed the correlation between degree of restriction of diffusion and tumour aggressiveness (Gleason score) and the sensitivity of the diffusion was 62% and the specificity was 90%. In a further 10 studies, the combination of T2-weighted images and diffusion gave a sensitivity of 76% and a specificity of 82%.
Dynamic contrast study: A contrast agent called gadolinium is injected intravenously and images of the prostate are taken every 2.5 seconds. Most prostate cancers show rapid contrast uptake compared to normal prostate tissue.
Spectroscopy: This reports on the relative concentration of metabolites in the prostate like citrate and choline. Citrate is a marker of normal prostate tissue, whereas an increase in the concentration of choline is suggestive of cancer. There is usually a correlation between the choline-citrate ratio and the aggressiveness of the tumour. Spectroscopy is the most sensitive NMR technique for diagnosing prostate cancer (92%) and has greater specificity than T2 imaging.
Pi-Rads Diagnostic Injury
All the parameters from the various tests are collected in a score from 1 to 5 (PI-RADS system) where lesions 1 are benign, 2 are possibly benign, 3 are dubious, 4 are possibly malignant, and 5 are very possibly malignant. Therefore, patients with PI-RADS lesions 4 and 5 should be biopsied and those with lesions 3 should be closely monitored.
Transrectal biopsy in prostate cancer
It is the most widely used method of prostate gland biopsy. Six samples from each prostate lobe are obtained, aided by ultrasound, through the rectum. A biopsy should be performed if there is suspicion of a tumour in the rectal examination (nodules or indurations in the prostate) or in cases with a PSA elevation greater than 4 or even greater than 3 in men younger than 50 years after having ruled out other prostatic causes which may explain the elevation of PSA (infections, inflammation, benign growth, etc.). The most common complications of prostate biopsy are haematuria, (blood in the urine), rectal haematuria, urine retention or fever from urine or prostate infection (acute prostatitis).
In men with PSA between 4 ug / L and 10 ug / L the chance of finding cancer with the first 12-cylinder biopsy is 40-45%. In 10% -20% of cases with the first negative biopsy, a second biopsy will show prostate cancer, while a third biopsy will show cancer in only 10% of patients.
Transperineal biopsy with template: the brachytherapy technique
In order to reduce the percentage of false negative cases (men with negative biopsies but who have cancer), other forms of prostate biopsy have been tried, such as trans-perineal biopsy using the brachytherapy technique. This maps the entire prostate, obtaining Between 20 and 30 cylinders from each prostate lobe under general anaesthesia or spinal anaesthesia.
Cancers detected with this technique tend to be smaller and of lesser extent. In patients with three or more negative biopsies, the percentage of positive biopsies with the brachytherapy technique becomes close to 50% of which half have been Gleason 7 and 14% Gleason 8 or greater. Only 11% of the cases had potentially insignificant tumours.
There is a greater percentage of complications with a biopsy with brachytherapy technique than with a transrectal biopsy, such as the possibility of urinary retention that requires a bladder catheter. The percentage of infection and sepsis is lower when a biopsy is not performed by the transrectal route. There is also no alteration in sexual function.
The increase in the number of cylinders obtained with a trans-perineal biopsy enables the urologist to detect tumours located in the anterior area of the prostate, which cannot be reached by the usual technique of transrectal prostate biopsy. This technique allows diagnosing between 30 and 40% of cancer patients who would not be diagnosed with a conventional prostate biopsy.
The limitation of this technique is that it must be performed with spinal or general anaesthesia. In case of a previous negative conventional biopsy, detection with the brachytherapy technique is 55%, with two negative biopsies being 42% and with three previous negative biopsies, 34%. With a biopsy with the brachytherapy technique, all the lesions observed in the multi-parameter NMR can be reached.
Read more: Brachytherapy for prostate cancer
Prostate biopsy with image fusion
The newest technique to detect prostate cancer combines the images obtained with a multi-parametric Nuclear Magnetic Resonance and the images obtained in the transrectal ultrasound in real time, using a computer program to direct the needle towards the lesions found suspected of malignancy PI-RADS 4 and 5. With this technique, the need for biopsies in men with PSA elevation decreased by 51%, the diagnosis of low risk cancers decreased by 89%, and the detection of intermediate and high risk cancers increased by 18% compared to biopsies obtained with transrectal ultrasound alone.


