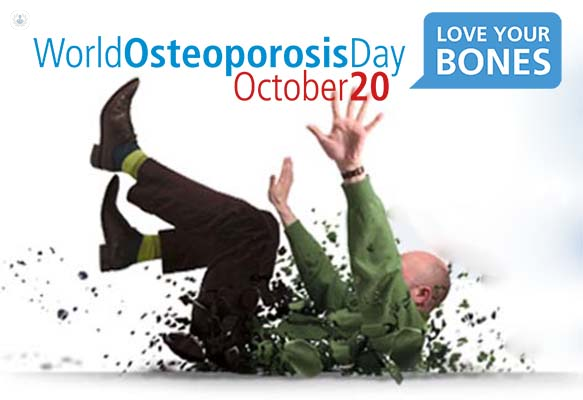
Don’t let osteoporosis fracture your future - 4 key questions answered by an osteoporosis specialist
Written by:As part of World Osteoporosis Day on 20th October, we asked consultant endocrinologist and expert in osteoporosis, Professor Gordana Prelevic to give her advice on how to strengthen your bones and avoid osteoporosis, and how to avoid fractures in those that already have osteoporosis.
1. Who is more at risk of osteoporosis?
Osteoporosis is a common condition in which bones become weaker and less dense, and as a result more likely to break (or fracture). It is most commonly found in women but men can also have osteoporosis as bone density diminishes for everyone with age. People with osteoporosis can suffer bad and life-threatening fractures from a minor slip or fall. More than a third of women and one in 12 men will suffer an osteoporotic fracture in a lifetime.
Risk factors for low bone density and osteoporosis are:
- age
- sedentary lifestyle
- early menopause
- irregular or no periods
- low body weight
- a family history of osteoporosis
- excessive alcohol or caffeine intake
- smoking
- long-term use of certain medications (steroids, antiepileptic drugs, anti-oestrogens, thyroxine, omeprazole, fluoxetine etc.)
- certain diseases (malabsorption, liver disease, thyroid disease, rheumatoid arthritis, hypogonadism in men, chronic kidney failure).
Those patients who have had a previous fracture, whose parents have had a hip fracture, or who have an increased likelihood of falling, have a higher risk of suffering a fracture. Why not take this osteoporosis risk test, 19 questions to test your bone health.
2. What are your tips for a healthier lifestyle and diet to help reduce the chance of osteoporosis?
Nutrition has a very important role in the prevention and treatment of osteoporosis. It has been shown that increasing calcium intake by increasing consumption of calcium-rich dairy products enhances bone development during childhood and adolescence.
Healthy eating habits are best established early in life. It is essential to encourage younger age groups to eat plenty of calcium-rich foods and drink milk to maximise bone density by the age when their peak bone mass is reached (about the age 23-25 years).
Eating healthily and doing exercise,
particularly during our teenage years before our bones are fully developed can help achieve peak bone density.
Physical activity
is really important for keeping your bones healthy and strong, especially weight-bearing exercise. Exercise is very important in helping to improve muscle strength, balance and flexibility, which can help prevent falls and fractures.
Milk and dairy products
are the major sources of calcium in the British diet. It is of great importance that those with a low calcium intake increase their intake of calcium-rich foods. Those at particular risk of low calcium intake are adolescents, young women and elderly women. The recommended calcium intake is 1000 to 1500 mg per day (a small glass of milk is around 300mg of calcium).
Vitamin D
has an important role in the development and maintenance of healthy bones. Eggs and oily fish contain good amounts of vitamin D. Everybody needs vitamin D supplements during winter months – especially here in the UK. This is particularly important for housebound, elderly people and women who wear traditional clothing which covers most of their skin.
Excessive drinking of caffeine-rich beverages
should be discouraged – coffee, cola and tea all contain caffeine. Excessive alcohol intake accelerates bone loss and should be avoided.
If you are lacking sex steroids (oestrogen for women and testosterone for men) they should be replaced if deficient. A consultant endocrinologist can help test your levels.
3. What should you do if you are concerned about osteoporosis
If you think you might be at a higher risk of osteoporosis – for example, you have experienced irregular periods or have a family history of the condition or have been on long-term steroid treatment – you should speak to your GP.
Your GP may then refer you for a DXA scan, which is a painless, non-invasive procedure that helps to measure your bone density. Low bone density on a DXA scan, particularly if associated with any of the recognised risk factors for osteoporosis would be followed by a referral to an osteoporosis specialist.
4. How is osteoporosis treated, are there any new medications or treatments?
A healthy diet which is rich in calcium, vitamin D supplements and regular weight-bearing exercise are often the key to management of osteoporosis and maintaining bone density levels.
A reduction in fractures rather than an increase in bone density is the main goal of the treatment of established osteoporosis. Treatment of established osteoporosis can successfully prevent further fracture and improve the quality of life but has to be tailored to specific age groups.


