Waiting for orthopaedic surgery during COVID-19? How to prevent your symptoms worsening
Written by:Overall, the number of patients waiting for elective surgery continues to increase dramatically with over 4 million currently on NHS waiting lists. Projections towards the end of the year are similarly gloomy.
Restarting waiting lists is a huge logistic task, and this is impacting on the private healthcare services locally. The government has taken control of a large number of private providers operating capacity which clearly will have a negative impact on private patients waiting as well.
While the situation remains uncertain, Mr Sunny Deo, a leading consultant trauma and orthopaedic surgeon in Swindon, explains the simple but important measures you can take to mitigate the effects of prolonged waiting and avoid any worsening of your symptoms.

Minimising your symptoms
The majority of knee conditions requiring surgery have an activity-related component. This means some activities will aggravate symptoms. The easiest activity to consider is walking. The majority of patients with a significant knee condition will experience greater symptoms either at the time or in the hours following a period of activity based on one or more of the following:
- durations of walking
- walking pace
- terrain e.g. evenness of ground, inclines or stairs involved
Most people will therefore sub-consciously alter some of these, commonly by reducing walking distance and/or pace. Some people with knee conditions can walk comfortably but not jog or run; in this situation the solution to minimising symptoms is easier! As well as minimising symptoms you should aim to improve them too.
Improving your symptoms
There will be measures that will ease symptoms. These include the classic “PRICE” quintet of: Painkillers, Rest, Ice, Compression and Elevation.
Additional relieving measures include:
- Local massage and gentle warming of the symptomatic area. People often get confused about mixed message advice about cooling or warming the area, but in essence, if it works for you, do it.
- Measures that ease symptoms are known as alleviating factors. For the reasons noted above, weight loss is important if you are overweight. Painkillers containing opioids such as codeine, morphine or synthetic versions like tramadol should be taken under medical supervision and discussion. Simple painkillers such as paracetamol can be taken more regularly.
- The other major group of painkillers are the non-steroidal anti-inflammatories (NSAIDs) such as ibuprofen, diclofenac, naproxen, and gain prolonged use of more than a week should be discussed with your GP as they can cause side-effects. All of these are useful in reducing or minimising symptoms.
- Use of a knee support. This has developed a bad reputation in the medical and physiotherapy spheres historically, but can be really useful. Again it is quite individualised, and some people do find it either aggravate local knee pain, causes swelling below or skin irritation. However if you think it helps, particularly for specific activities i.e. allows you to walk that mile comfortably, than use it! You can pick up a standard knee support for a decent sized pharmacy.
Avoid aggravating activities
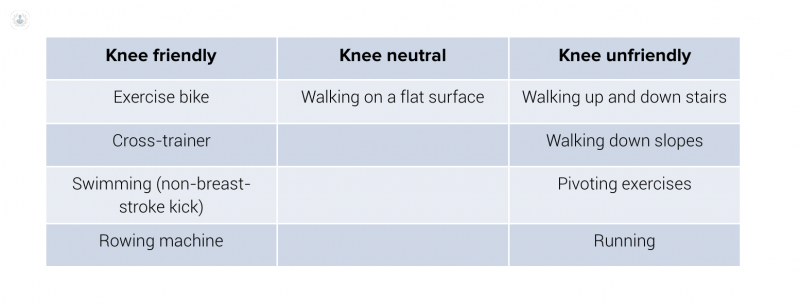
The more knee unfriendly activities you do, the worse your symptoms will become.
In general, activities involving weight-bearing tend to cause most problems. Also, the less you do, the less it’ll hurt; lots of people find their knee symptoms improve when they go on (a relaxing beach) holiday. There is a fairly obvious snag in this advice, and that’s because we do an awful lot of stuff upright and we all need to walk at least a bit. Lots of people will have jobs or pastimes involving walking. Any activity that flares symptoms is known as an aggravating factor; these are best avoided.
When you load your joints, you create forces across them. These are called the ground reaction, and at the front of the knee. Activities such as stair climbing and running put a much larger force through the front of the knee than walking, but that even walking on the flat this generates ground reaction forces up to 1.4x your body weight for every step you take. Non-impact exercises such as low-resistance cycling, using a cross-trainer, swimming, walking in water and rowing put lower forces through the front of the knee joint, for the equivalent amounts of aerobic energy expended and muscle work done.

It also means there is a direct effect of body weight on forces across the knee joint, and the importance of weight loss to optimise your body weight prior to surgery, if this is relevant to you.
The impact of exercise will also be modulated by the strength and conditioning of your muscle groups and you exercise history. This creates a scale of exercising which puts less or more force through the knees and therefore a scale of “friendliness” of certain exercise types can be seen.
Muscle conditioning
Optimising muscle strength is a really important factor in relieving symptoms.
The most important muscle groups for the knee and the big ones at the front (quadriceps) and back (hamstrings) of your thigh. People with excellent muscle strength and conditioning will be able to undertake knee unfriendly exercise with less chance of generating symptoms. One can essentially consider the muscles above and below the knee to be acting as shock absorbers for the knee joint; the weaker those muscles, the more load goes through the knee.
Unfortunately one of the key effects of having a painful knee condition is it causes muscle deconditioning; in some patients, this can be quite severe.
To minimise your knee symptoms you need to try and avoid knee unfriendly exercise and undertake as much knee-friendly exercise as possible. How much exercise do I need? This is very individualised, but the general rule is if it causes symptoms you’ve done too much.
Remember as a society we do far less exercise/activity than we should, so as long as it doesn’t cause symptoms, the more the better. It should help with building and strengthening muscles and might help weight loss.

This does not much help people who do a lot of housework, walk to work, have physical jobs or need to walk their dog. This is difficult, but the keywords here are pacing and prioritisation.
If your symptoms start after one mile of walking, do several shorter walks. The same goes for household or gardening activities. For work, a discussion with your line manager is likely, but it should be in your company’s interest to keep you as well as possible in the lead up to surgery as this will optimise your chance for a smooth recovery. Prioritisation means that at the start of a day when the knee doesn’t feel too bad, avoid the temptation to do loads of stuff; do the most important and ensure symptoms aren’t flaring before undertaking something else.
Additional treatments
-
Cortisone injections
These are the traditional mainstay of alleviating pain and inflammation from a joint without surgery. However, repeated cortisone injections are not recommended, and in general, if you have severe osteoarthritis with bone on bone wear out, the likelihood of them working for more than a few weeks is limited.
If you have had little or no benefit from a cortisone injection for over two months duration, the likelihood is further repeated injections are not going to help you. There have also been concerns raised about the use of cortisone into joints with COVID-19, and the general advice is to use the lowest possible dose, and only if necessary.
The local effect of cortisone to the bone in severe arthritis where the joint surface is completely worn away is a major cause for concern, in conjunction with the likelihood of the injection working being very low at only 10% or so. This local effect often causes local softening of the bone and therefore can lead to a more rapid progression of arthritic wear out.
-
Knee Bracing
Certain knee problems, particularly single compartment arthritis or single ligament injuries have specific braces designed for the condition and can help some patients regain a greater degree of symptom-free function. You will need to see a specialist doctor or physiotherapist to prescribe and fit these types of brace and they are expensive.
-
Hylan / hyaluronic acid / viscosupplementation injections
These products are not cortisone based and are the glycoprotein substance that acts as an anchoring point for the collagen protein and water molecules in normal joints. There are a number of injection types in current use, and the one I have the most experience in using over the past 10 years in Synvisc 1, but I’ve also used Fermathron S, Durolane and Ostenil. Although often marketed and described as lubricating fluid, I see them as a synthetic joint surface.
In the presence of end-stage arthritis where the joint surface is completely worn to the bone, its usefulness drops as the hylan has less to stick to. However, there will be a percentage of patients in whom this product may well improve symptoms significantly for a few months without the potentially detrimental effects of cortisone on barebone within a joint. If started prior to complete wear-out, hylan can be used repeatedly to reduce arthritic pain and possibly slow arthritic progression. I have a small group of patients who I’ve been injecting annually for over a decade, with no ill effects thus far.
-
Platelet-rich plasma injections
This group of injections is the newest type of “biologic” injection, and again it's not been subject to large cohort studies, but in selected patients and certainly, for sports injuries, the resolution times for symptoms and healing are often really good.
Its role in osteoarthritic conditions is still to be defined, and it's likely that once the joint is completely worn out, with bone on bone, injection efficacy will drop to less than 40% effectiveness in terms of symptom reduction and improved function.
It is however very safe, as the plasma is your own! A blood sample is taken, centrifuged, the plasma layer selectively removed and injected into the knee.
If you want to discuss or enquire about any aspect of this information, including non-cortisone joint injections, do not hesitate to contact Mr Sunny Deo through his Top Doctors profile.
References:
Denham RA & Bishop RAD Mechanics of the knee and problems in reconstructive surgery. J Bone and Joint Surg., 60B, 345-8. 1978.
Goodfellow J, Hungerford DS, Zindel M. Patello-femoral joinr mechanics and pathology. J Bone and Joint Surg., 58B, 287-299. 1976.
DD D’Lima et al. Knee joint forces: prediction, measurement, and significance. Proceedings of the Institute of Mechanical Engineers. Section H: Journal of Engineering in Medicine. Feb 226(2) 95-102. 2012.


