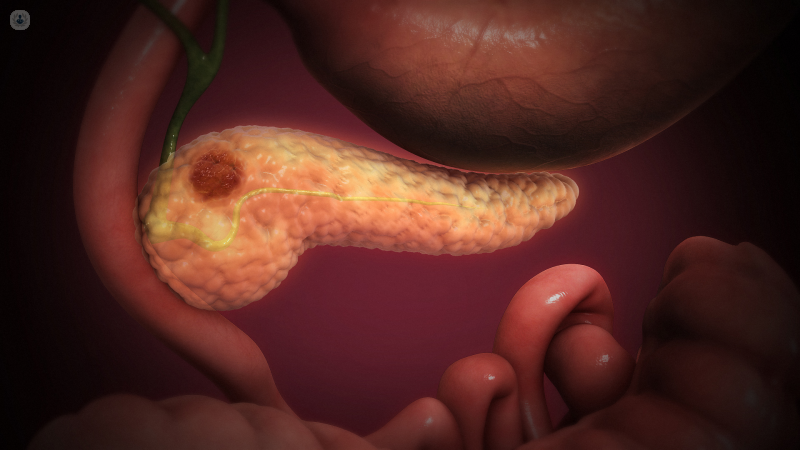
Pancreatic cancer: your treatment options explained
Written by:Treatment for pancreatic cancer has improved significantly in recent years, so which is now the most effective option? In this up-to-date guide, leading surgeon Mr Nicola de’ Liguori Carino explains the different options available today, from traditional techniques such as surgery, radiotherapy, and chemotherapy, to brand-new therapies such as irreversible electrocorporation (IRE).
Surgery
Surgical resection, i.e. cutting out the cancer, is the only treatment that can offer a chance to cure pancreatic cancer. Current scientific evidence from large international multicentre randomised trials (studies where patients are randomly assigned to receive one treatment or the other) show a significant increase in survival when curative surgery is followed by chemotherapy (adjuvant chemotherapy).
Unfortunately, at presentation, 80% of patients with pancreatic cancer are not surgical candidates due to the presence of metastatic (50%) or locally advanced disease (30%).
Pancreatic cancer that affects any major blood vessel but has no evidence of distant metastases (where the cancer has spread to other parts of the body) is classified as stage III. If distant metastases are present it is classified as stage IV pancreatic cancer.
According to the degree of infiltration of the cancer into major blood vessels surrounding the pancreas, stage III pancreatic cancer is further divided in to 2 categories:
- Borderline resectable pancreatic cancer (BRPC)
- Locally advanced pancreatic cancer (LAPC).
While resection could be attempted in borderline resectable pancreatic cancer, locally advanced pancreatic cancer (LAPC) is inoperable due to encasement of blood vessels that can’t be removed or reconstructed. In this case, other treatment options will be considered.
Chemotherapy
The standard of care for LAPC is systemic chemotherapy, with the goal being to downstage the tumour (shrink it, freeing it from unresectable major blood vessels), thus potentially making it resectable. However, this is relatively infrequent, with only up to 30% of patients achieving this result.
If with systemic chemotherapy the disease remains stable, without local progression (growth of the tumour size) or development of metastases, local treatment with radiotherapy and/or irreversible electroporation could be considered.
Radiotherapy
In stage III LAPC, both radiotherapy and irreversible electroporation aim to stop the growth of the tumour by killing the cancer cells. This prevents it from releasing further cancer cells into the bloodstream, which is the cause of progression into stage IV pancreatic cancer with metastatic disease.
Radiotherapy (with or without simultaneous low dose of chemotherapy, known as chemoradiotherapy) has been used in this setting for a longer period of time than IRE, showing some potential benefits in helping to control tumour growth and reducing some of the symptoms caused by pancreatic cancer. However, there is no clear evidence that radiotherapy will increase overall survival. Nevertheless, chemoradiotherapy in patients with no progression while on systemic chemotherapy has been shown to maximise local control and improve treatment-free survival.
Irreversible electrocorporation (IRE)
Since irreversible electroporation is a relatively new technique, the evidence to support its use in pancreatic cancer is still very weak. In fact there are contrasting results, making it difficult to draw clear conclusions on its potential advantages. Some studies seem to indicate that patients who underwent IRE after systemic chemotherapy were more likely to survive for longer, while other studies did not report any survival advantage.
Currently, a number of international randomised trials are taking place to determine if IRE in LAPC is superior to chemoradiotherapy. Results are still awaited.
In May 2017, the National Institute for Health and Care Excellence (NICE) of the United Kingdom released updated guidance for the use of IRE in the treatment of patients with pancreatic cancer. It states that current evidence on the safety and efficacy of irreversible electroporation for treating patients with pancreatic cancer is inadequate in quantity and quality. Therefore, this procedure should only be used in the context of research.
In fact very few centres and experts in the UK, including our in Unit in Manchester, currently offer irreversible electroporation for pancreatic cancer.
In essence, because of the above facts, we strongly believe that IRE should only be offered for stage III locally advanced pancreatic cancer to those patients without a significant decline in their health during their chemotherapy, possibly followed by chemoradiotherapy, and who have stable disease on completion of this treatment. IRE, like radiotherapy, is definitely not indicated for stage IV pancreatic cancer where distant metastases are present. In this setting IRE would only produce potential side effects, including possible decline in general health, without offering any survival advantages.
Read more: irreversible electrocorporation (IRE)
Visit Mr de’ Liguori Carino’s profile to learn more or to book an appointment.


