Neuropathic pain: causes and treatment
Written by:Neuropathic pain is pain that one suffers from as a direct consequence of previous damage and/or disease that has adversely affected the somatosensory system.
In our latest article, highly revered pain management specialist, Dr Basil Almahdi, explains in-depth what exactly neuropathic pain is and how it is caused, whilst also revealing whether or not this specific type of pain may be a sign of a more serious underlying condition.
What is neuropathic pain and how is it caused?
Neuropathic pain is pain caused by a lesion or disease of the somatosensory system, or, in other words, pain initiated by a dysfunction in one’s nervous system. It presents as a combination of positive and negative phenomena.
The positive phenomena include various painful symptoms, paraesthesia and/or dysesthesia, which, by definition, are abnormal non-painful sensations (e.g., tingling, numbness, and/or pins and needles). Negative phenomena usually include neurological sensory deficits in the painful area, together with other deficits (motor, cognitive etc.), depending on the location of the lesion.
What are the most common neuropathic pain presentations?
There are some commonly used terminology phrases that are used to describe neuropathic pain presentations, with the main ones being as follows:
- Spontaneous pain: shooting, burning, stabbing, or electric shock-like pain, tingling, numbness, or a “pins and needles” feeling
- Evoked pain: pain brought on by normally non-painful stimuli such as cold, gentle brushing against the skin, pressure, etc. This is referred to as allodynia. Evoked pain may also imply an increase of pain by normally painful stimuli such as pinpricks and heat. This type of pain is called hyperalgesia.
- An unpleasant, abnormal sensation whether spontaneous or evoked (dysesthesia).
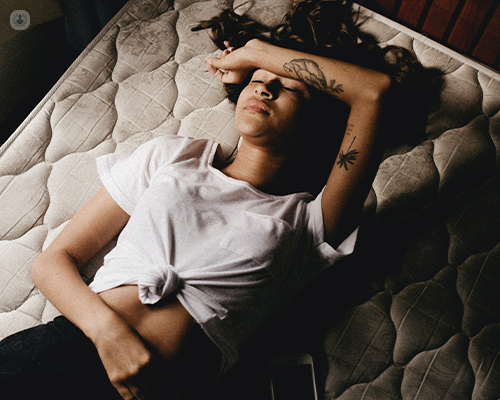
- Trouble sleeping, and emotional problems due to disturbed sleep and pain.
- Pain that may be lessened in response to a normally painful stimulus (hypoalgesia).
Is neuropathic pain a sign of an underlying condition?
It is important to know that neuropathic pain is a presentation of an underlying disease or dysfunction rather than a disease itself. More often than not unfortunately, the underlying cause cannot be found or isolated.
Peripheral neuropathic pain: what are the main causes?
Neuropathic pain represents a broad category of pain syndromes encompassing a wide variety of peripheral and central disorders. Thus, it can either have a peripheral or central aetiology.
Examples of peripheral neuropathic pain include painful diabetic peripheral neuropathies, post-herpetic neuralgia, and traumatic nerve injury. However, the commonest cause of peripheral neuropathic pain is that caused by compression at the spinal nerve root, referred to as radiculopathy. This type of pain possesses both neuropathic and non-neuropathic components.
What causes central neuropathic pain?
The central causes of neuropathic pain are much less common than the peripheral causes. Stroke pain is observed in up to eight per cent of patients after a stroke.
In spinal cord injury, up to 50 per cent of patients may develop neuropathic pain, mainly related to the development of syrinx in the middle of the cord. Multiple sclerosis is another cause of central neuropathic pain, with up to 25 per cent of MS patients typically presenting with this type of pain.
What about non-neurological causes?
Systemic illness or chemical toxins are responsible for a large proportion of neuropathic pain syndromes. The commonest cause of neuropathy is diabetes mellitus, which accounts for up to 30 per cent of all neuropathy presentations. Other causes include alcoholism, HIV disease, chemotherapy and radiotherapy-related pain.
How is neuropathic pain treated?
Whenever possible, treatment of neuropathic pain should be directed first at the removal or treatment of the underlying cause. Effective treatment would typically involve the removal of the compressing lesion onto the affected nerve, or better management of the blood sugar level in diabetes.
Multimodal therapy (including medicines, physical therapy, psychological counselling and sometimes surgery) are all other extremely effective treatment options and are all usually required to treat neuropathic pain.
The pain can also be treated with nerve blocks given by pain specialists, including injections of steroids, local anaesthetics, or other medicines into the affected nerves. Neuropathic pain that has not responded to the therapies mentioned above can be treated with spinal cord stimulation, peripheral nerve stimulation as well as brain stimulation.
Like every other chronic pain condition, it is vital to approach the management of neuropathic pain problems in a multidisciplinary approach. Chronic pain problems have a multifaceted bio-psycho-social impact on the patient’s life. Therefore, input from an experienced physiotherapy team and psychology team is pivotal in the management of these cases.
What are the main treatment goals?
The main objectives of treatment for neuropathic pain include the following:
- to treat the underlying disease (for example, radiation or surgery to shrink a tumour that is pressing on a nerve)
- to provide pain relief
- to maintain functionality
- to improve quality of life
Why is it essential to see a specialist?
As the neuropathic pain can have such a variety of causes and predisposing factors and is treated with such a variety of medications and interventions, it should always be treated under the supervision of a specialist. This allows the patient to have a full assessment and approach management in a holistic way to be able to treat such a complex, multifaceted problem successfully.
Dr Basil Almahdi is a highly experienced and renowned London-based pain management specialist who specialises in neuropathic pain. Book a consultation with him today by visiting his Top Doctors profile today.


