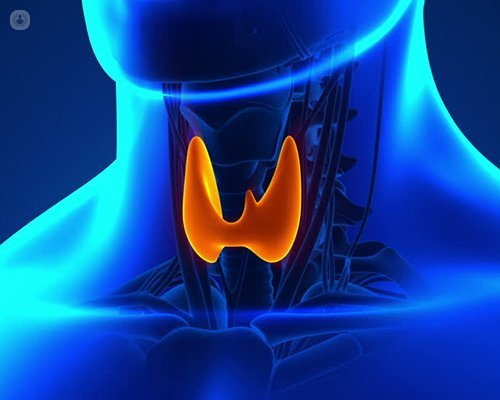
Thyroid and parathyroid surgery explained
Written by:The thyroid gland is located in the lower neck. Its function is to control our body’s metabolism or how much “fuel” we burn, and acts like the accelerator pedal of a car. The thyroid produces a hormone called thyroxine, without which our bodily processes slow down and normal health of our tissues is affected. This can lead to changes in the skin, hair and even how our brain functions. The parathyroid glands are glands at the back of the thyroid hence their name. They help control our calcium level.
Why is thyroid or parathyroid gland surgery needed?
The thyroid gland can become overactive, develop nodules or lumps which grow causing a large thyroid gland known as a goitre or sometimes the nodules or lumps are cancerous. To treat these problems patients may require removal of the thyroid gland known as thyroidectomy.
Thyroid surgery involves removing half or all of the thyroid gland. The length of the operation can be anything from 30 minutes to two hours depending on the complexity.
Parathyroid gland surgery
Occasionally, one or more of the parathyroid glands can become overactive which leads to calcium being taken out of the bones resulting in a high calcium level known as hypercalcaemia.
Patients with hypercalcaemia will be referred for surgery to remove the offending gland or glands to restore a normal calcium level.
80% of parathyroidectomy surgery involves removal of just one gland, but occasionally all four glands have to be inspected to allow abnormal glands to be identified and removed.
Parathyroid surgery can take between 20 minutes or two hours again depending on patient factors and case complexity.
What are the risks of thyroid and parathyroid surgery?
As in all surgery, bleeding and infection are the most common but nonetheless rare complications. Damage to the voice box nerve and a need for long term vitamin D and calcium can also occur in less than 5% of patients.
Complications are related to surgical experience and the annual volume of surgeries the surgeon performs. Complications are higher if surgeons perform less than 30 thyroid and 50 parathyroid operations each year.
The risks of parathyroid surgery are similar to those of thyroid surgery but less common. There is no guarantee that patients will be cured after their first operation. Surgeon experience and expertise is particularly relevant to the probability of a successful outcome with low risk of complications.
What is the procedure for thyroid and parathyroid surgery?
The most common and conventional approach is to make an incision in the neck. Recent pioneering techniques involve robotically-assisted surgery, where an incision is made in the armpit rather than the neck to avoid a neck scar. It is not suitable for all patients though.
In focused parathyroid surgery a small 2cm incision is made in the neck which enables a preoperatively identified parathyroid gland to be removed. It again is not suitable for all patients. The gold standard operation still remains a four gland parathyroid exploration. The latter involves a larger incision of approximately 4cm.
For the best results for this kind of surgery, it is always advisable to check the registry of surgeons on The British Association of Endocrine and Thyroid Surgeons (BAETS) where the number of procedures carried out by a surgeon is recorded.


