Tracheoesophageal fistula in adults: what are the causes, and how is it treated?
Written by:A tracheoesophageal fistula (TOF) is an abnormal connection between the trachea (windpipe) and the oesophagus (gullet).
Tracheoesophageal fistulae are either congenital or acquired, with congenital fistulae being more common and presenting shortly after birth, and are treated by paediatric surgeons. This article is about the presentation and treatment of acquired tracheoesophageal fistulae in adults.

What causes acquired tracheoesophageal fistula in adults?
The oesophagus is in contact with the trachea along the entire length from the neck to the mid chest. A fistula can arise at any level along this area of contact. In adults, the vast majority of TOFs are acquired due to a number of conditions.
These include malignant conditions of the trachea, such as oesophageal tumours and tissue necrosis caused by them and trauma from interventions to the trachea or the oesophagus such as stenting of the oesophagus and tracheostomy. TOFs are increasingly seen as a complication of often successful treatment of oesophageal malignancy for instance with chemoradiotherapy and stenting.
What are the symptoms of tracheoesophageal fistula?
If the TOF is tiny, there may be no symptoms, however if the fistula is large enough to allow saliva or fluid to pass from the oesophagus into the trachea, the presentation will be with a recurrent cough particularly on eating and drinking as well as recurrent chest infections.
The TOF can be diagnosed with radiological imaging, either with a contrast swallow or CT scan as well as with bronchoscopy.
How is tracheoesophageal fistula treated?
The treatment depends on the underlying cause of the TOF, as well as the site and size of the fistula. TOFs are rare and require the expertise of a multidisciplinary team to achieve the best outcomes. The skills required include the expertise of interventional gastroenterologists, respiratory physicians, thoracic and UGI surgeons.
The ideal treatment for a TOF is to surgically close it, ensuring that the underlying disease is also treated. The operations can be technically challenging, requiring experience in operating on the trachea and oesophagus as well as the ability to reconstruct the oesophagus using the stomach or the colon. High TOFs also require the expertise of being able to operate in the neck and ensure that there is no damage to the nerves supplying the vocal cords.
There are very few centres in the UK that have the expertise in treating TOFs. To make an appointment with a tracheoesophageal specialist, click here.
Case studies of patients with tracheoesophageal fistula
Patient A
This patient presented at the age of 29 with a few years 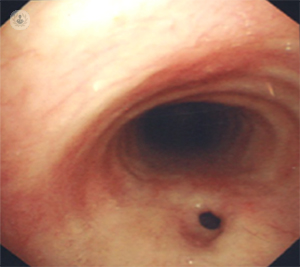 history of symptoms that were thought to be due to asthma. When treatment for asthma did not result in an improvement, she underwent further investigations including a CT scan which showed a small TOF situated at the root of her neck. She underwent an assessment of this with a bronchoscopy and oesophaguscopy following which an operation was performed through the neck closing the fistula and interposing muscle tissue between the separated oesophagus and trachea. She made a straightforward recovery and was discharged a week later with her symptoms resolved.
history of symptoms that were thought to be due to asthma. When treatment for asthma did not result in an improvement, she underwent further investigations including a CT scan which showed a small TOF situated at the root of her neck. She underwent an assessment of this with a bronchoscopy and oesophaguscopy following which an operation was performed through the neck closing the fistula and interposing muscle tissue between the separated oesophagus and trachea. She made a straightforward recovery and was discharged a week later with her symptoms resolved.
Patient B
This patient was known to have a condition called 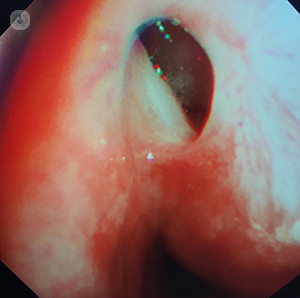 scleroderma which affects the oesophagus and results in difficulty with swallowing. She presented with a worsening of her swallowing at the age of 55 and underwent an endoscopy. This showed an abnormality in the oesophagus which was biopsied and the pathology report showed a B cell lymphoma. She had successful chemotherapy for this but unfortunately developed a TOF as a consequence.
scleroderma which affects the oesophagus and results in difficulty with swallowing. She presented with a worsening of her swallowing at the age of 55 and underwent an endoscopy. This showed an abnormality in the oesophagus which was biopsied and the pathology report showed a B cell lymphoma. She had successful chemotherapy for this but unfortunately developed a TOF as a consequence.
She underwent a closure of the fistula along with the removal of the oesophagus which was diseased, and a subsequent reconstruction which involved making her stomach into a tube which was then taken up to the neck underneath the breastbone and joined to the healthy remaining oesophagus in the neck. Although she developed a leak from the join in the neck, this eventually healed and she is now able to swallow properly and has been cured of her fistula.



