Trigger finger: causes, symptoms and treatment
Written by:Trigger finger is a common condition that can affect any of the fingers at any age, which means it can occur in both children and adults. This article, however, will focus on trigger finger in adults.
Trigger finger can lead to stiffness, pain, clicking, triggering or locking of the fingers. One of our leading orthopaedic surgeons Ms Anna Moon explains the causes, symptoms and both the non-surgical and surgical treatment options of the condition.

What causes trigger finger?
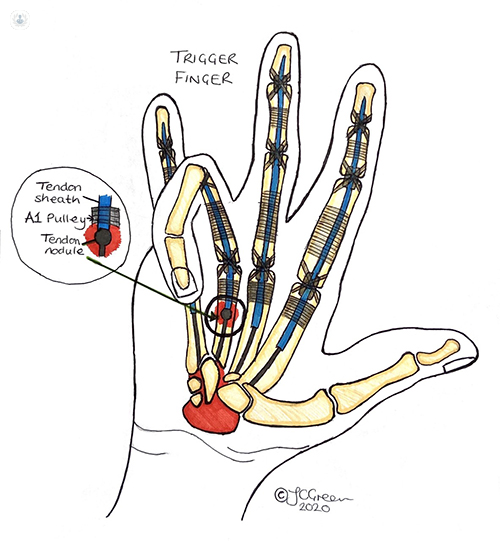
Normally, the tendon known as the flexor tendon pulls the finger so it glides towards the palm when you make a fist. In cases of trigger finger, this tendon does not glide easily and your fingers can become stuck in a bent position making it difficult to make a fist. They may bend or straighten with a snap, like a trigger being released.
Trigger finger is caused by the jamming of the flexor tendon in the entrance of the tendon sheath (or the A1 pulley), which could be inflamed and thickened. The flexor tendon itself may also be swollen.
The condition can happen spontaneously and is common in those who are middle-aged, particularly women. It is also associated with diabetes and there is a higher incidence and recurrence rate in diabetic patients.
Finger trigger could also be caused by a sharp, penetrating injury to the flexor tendon making the normally smooth tendon surface uneven and catching on the tendon sheath.
What are the symptoms?
The fingers feel stiff if you try to make a fist or bend them. Bending the fingers takes more effort as they are tender and painful. There may be a popping/ clicking sensation when moving the finger. As the imbalance between the tendon and the opening of the tendon sheath is increasing, the fingers lock into a bent position. You will need to use the other hand to unlock the finger because it has become stuck.
How can trigger finger heal?
Trigger finger can settle on its own. If it progresses further with clear triggering and locking of the finger that is painful, we may recommend the following during its early stages:
- Activity modification and night splinting in extension
- Non-Steroidal Anti-inflammatories (NSAIDs)
- Hand therapy - including tendon gliding hand exercises
- Splinting - with a specific one to be worn known as a relative motion splint
- Steroid injections
In cases of persistent or recurrent symptoms, we consider surgeries. In diabetic patients recurrence is common and they are likely to end up having surgery.
What are the surgical options?
There are two surgical options for trigger finger release. The most common procedure is an open release using a small incision to release the A1 pulley. Sometimes we perform a percutaneous release, where we release the A1 pulley with a needle. Both procedures are performed under local anaesthetic.
What happens after surgery?
The stitches remain in situ for two weeks following surgery and will then be removed. There are not many restrictions post-operation but it is important to keep the hand elevated to reduce the swelling. It is also recommended to move the fingers straight away to keep them mobilised so that the tendon does not get stuck to the surrounding tissue.
When should I visit a doctor?
Most patients go to their GP where they can get their diagnosis of trigger finger. Some GP surgeries do an in-house steroid injection or patients could be referred to a hand surgeon.
Worried that you’re living with trigger finger? You can make an appointment to see Ms Moon via her Top Doctor’s profile here for her expert opinion.


