What do interventional radiologists do and what can they offer the patient?
Written by:Dr Ian McCafferty is a leading interventional radiologist and here he explains exactly what interventional radiologists do and how their specialised treatments can offer patients a choice of treatment options.
In this article I would like to take you on a journey to know what an interventional radiologist (often called an IR) is, and what treatments we can offer patients. Although IR can offer solutions in many areas of medicine, I am going to concentrate in this article on what we can offer in the management and treatments for cancer. These treatments are the youngest and most rapidly growing area of IR that is often referred to as interventional oncology (IO) – the fourth pillar of cancer treatment and palliation.
What is interventional radiology?
One of the first questions I am often asked by patients, and to be honest some doctors, is “what is interventional radiology?”. To me this is a major problem that primarily affects the patient’s ability to discover the fantastic image guided therapies that are at the forefront of medical technology and innovation for their conditions. It is also a cause for concern that we as interventional radiologists have failed to educate the public regarding our skills and treatments we offer since the birth of IR in the late 1960s. To this end we as interventional radiologists are also now known as image-guided surgeons.
Interventional radiologists are doctors that have had specialist training in the interpretation of imaging techniques such as CT, MRI and ultrasound scans and the use of imaging to guide special tubes, needles and guidewires to the area of interest though 3-5mm incisions in the skin. This means that patients avoid a significant number of risks related to open and laparoscopic surgery with significantly faster recovery times. Most treatments in IR can be done as a day case with rapid recovery and are revolutionising cancer treatments and palliation.
What can interventional radiologists offer patients?
IRs specialising in interventional oncology can help improve the quality of life of patients with cancer in a number of ways. On a simple level IRs can provide access to veins to allow the administration of chemotherapy, this can be done with tunnelled lines (Hickman, Groshong & Broviac lines) or more recently with Ports / Powerports. Ports are implanted devices that allow access for blood tests, chemotherapy and dye for CT scans. They are unobtrusive, hidden, easy to access and prevent all the hassle of multiple cannulas when attending for chemotherapy. IR can also sample an abnormal area with an image guided biopsy to make a diagnosis as well as help when patients run into difficulty, for example, blockages in the drainage of kidneys, liver and central veins where we can relatively easily place special plastic and metal stents to hold these tubes open and restore normal function, thereby improving quality of life.
How can interventional radiologists treat cancer?
On a more complex level, IRs can be actively involved in the primary treatment and cure of certain cancers and in the active management of metastatic disease especially in the liver and lung. There are broadly speaking two distinct techniques used by IRs in this regard: percutaneous thermal ablation and embolisation techniques. Both techniques are image-guided, using small needles and tubes (catheters) to target the cancer with the aim of causing cell destruction either with thermal energy or by blocking the small arteries that feed the cancer with embolisation or combined with chemotherapy agents or selective internal radiotherapy beads. Both techniques have been around since the 1980s but advances in the equipment to deliver the treatments has only happened more recently. Areas where these techniques have been used successfully include liver cancer (primary and liver metastasis); lung cancer (primary and lung metastasis); kidney cancer, bone cancer (primary and bone metastasis); prostate cancer and pancreatic cancer.
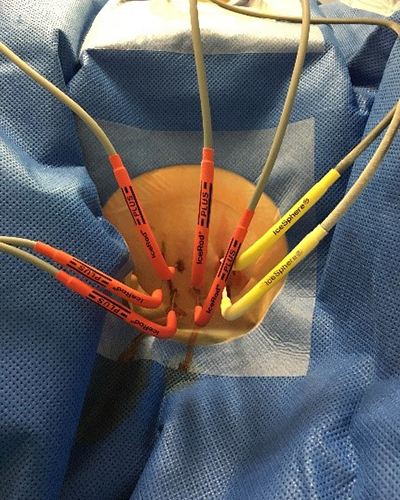
There are a number of different techniques used to impart thermal energy to cause cancer cell destruction and death. They all use the same image-guided method for the placement of the needles. The commonest are radiofrequency ablation (RFA) and microwave ablation (MWA) which work by heating the cancer cells to death; cryoablation (Cryo) which freezes the cancer cells to death and irreversible electroporation (IRE) which uses electricity to disrupt cancers cells to death.
Learn more about irreversible electroporation here!
In my next article, I will use examples of cancer in different parts of the body to help explain how the aforementioned treatments benefit the patient.
If you have recently received a cancer diagnosis and would like to discuss potential treatment options, make an appointment with an expert.



