What to expect when having lower GI surgery
Written by:There are various reasons a patient might undergo lower gastrointestinal (GI) surgery, as there are many diseases and conditions that can affect this part of the body. Experienced consultant general surgeon, Mr Greg Wynn, has clearly described the basics of lower GI surgery and has advised what to expect when having the procedure.
What is lower GI surgery and when might this procedure be recommended?
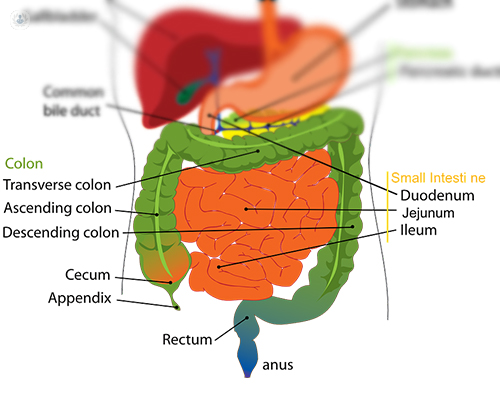
Lower GI surgery is any surgical procedure that involves the embryological mid- or hind-gut. This essentially involves most of your small intestine, colon, rectum, and anus. Diseases in each of these parts of the bowel cause different symptoms and have varying treatments, so it is always important to seek advice if you have a new issue or notice something isn’t quite right. Any new rectal bleeding, abdominal pain, change in bowel habit, or unexplained weight loss should be investigated. A new lump or swelling also requires an urgent assessment by a specialist.
Surgeons can perform lower GI surgery to have a look inside the abdomen to make a diagnosis or to remove diseased tissue when necessary. Sometimes this requires removing a section of bowel or removing a bowel appendage such as the gallbladder or appendix. Lower GI surgeons also operate on muscle weaknesses in the abdominal wall to fix hernias.
How is lower GI surgery usually performed?
These days, standard practice is for lower GI surgeons to use a minimally invasive or “keyhole” technique to perform most of their surgery. In the abdomen, this is known as laparoscopy and involves making tiny cuts in the skin to insert ports so that various keyhole instruments can pass through into the abdomen to work on the contents. One of these ports is used for a small camera and these images are transferred to a high-definition monitor so that magnified views can be obtained of the anatomy inside the body. Sometimes a keyhole approach is not possible. This can be because more complex work needs to be done or a large mass needs to be removed. In emergency situations it can be quicker to perform open surgery or sometimes the bowel is so distended that a laparoscopic approach is impossible. Either way, lower GI surgery is tailored to each individual so that they get a safe and effective solution to their problem.
How should someone prepare for lower GI surgery?
Different operations require different preparation, but usually clear instructions are given to the patient after a pre-operative clinic assessment. This pre-admission process a few weeks before the surgery is important to minimise the risk in the peri-operative period and make sure everyone understands what is planned and what is expected. For some operations, the bowel needs to be cleaned out with laxatives or there might be dietary restrictions. Patients will have to avoid eating food for six hours and drinking water for two hours before any surgery requiring a general anaesthetic.
What are the risks of this procedure?
Risks of lower GI surgery will depend on the size of the procedure and the medical fitness of the patient. The pre-assessment process will help to quantify the risks for you, and your surgeon should discuss the specific risks and benefits of the operation with you by making sure you understand the consent form and letting you have a copy of this. All surgery carries some risk, and these can vary from extremely rare but serious events to more common problems that are just a nuisance. Some of the common things that are mentioned on a consent form are: bleeding, infection, conversion from keyhole to open surgery, damage to surrounding structures, hernias, and clots in the legs and lungs (venous thromboembolic disease). Wound infections may be as high as one in twenty patients, whereas a clot in the leg might be as rare as one in tens of thousands for day-case procedures.
How long does it take to recover from lower GI surgery?
Many operations within the abdomen can be performed as day-case procedures, meaning a few hours after the surgery you will be in a safe condition to go home. It is important in this situation to have someone to take you home and support you for a day or two afterwards. For bigger operations, an in-patient stay is required to allow adequate pain relief to be given, assessment of normal post-operative checks to be carried out, and ensure that patients are eating, drinking, and mobilising adequately. Many of the benefits of keyhole surgery are seen in the post-operative period with less pain, quicker return to normal activities, and some specific complications such as hernias and adhesions being less frequently encountered.
Once home, post-operative recovery will depend on age, frailty, and the type of surgery in addition to whether there have been any complications. For example, atypical patient in their seventies may take up to three months to fully recover from a bowel cancer operation whereas a day-case laparoscopic groin hernia repair may only take a few days to recover from in a fit, young patient.
If you are having symptoms of a gastrointestinal problem, you can go to Mr Wynn's Top Doctors profile and schedule a consultation.


