Tendinopathy
Mr Mark Dunbar - Orthopaedic surgery
Created on: 05-07-2018
Updated on: 04-13-2023
Edited by: Sophie Kennedy
What is tendinopathy?
Tendinopathy is an umbrella term for diseases of the tendons. Tendons are fibrous cords of tissue that hold muscles to bone, and in order to do their job, they must be strong and flexible. Despite this, they can be injured due to overuse.
Tendinopathy broadly refers to three varieties of tendon injury, and is often confused with, or used synonymously with them. They are:
- Tendonitis/tendinitis – inflammation of a tendon, usually due to acute injury caused by overuse or repetitive strain.
- Tendinosis – chronic tendon injury with little or no inflammation, involving micro-tears in the affected tendon. Tendinosis causes long-term pain and is degenerative.
- Paratenonitis – inflammation of the outer sheath (paratenon) that surrounds certain tendons, such as the Achilles. There is some debate as to whether this should be considered separate from tendonitis.
All of these conditions increase the risk of a more serious tendon tear, or rupture.

What are the symptoms of tendinopathy?
The common symptom of all types of tendinopathy is pain in or around the tendon, most commonly in the place where it attaches to the bone. Other symptoms depend on the type of tendinopathy – for example, tendonitis is characterised by inflammation, including heat, swelling and redness, while tendinosis is a chronic ache, pain or stiffness without much, if any inflammation. The pain is usually worse during and after activity, and the area around the joint can be stiffer the following day.
There are tendons in many parts of our bodies, and tendinopathy can occur in any of them. It most commonly strikes in tendons such as those in the arms, shoulder, hands, and the Achilles tendon (in the heel).
What causes tendinopathy?
It is thought that the biggest factor in most tendinopathies is overuse, although there are many theories regarding other possible factors, such as thermal damage and load-induced ischemia. Both sudden bursts of exertion leading to injury and repetitive movements are thought to be the main causes of tendonitis, and obesity is thought to be a risk factor.
In the case of calcific tendonitis, calcium deposits in the tendon are the cause of the inflammation, but why they build up in the first place is not fully understood.
How can tendinopathy be prevented?
While it is impossible to prevent with one hundred per cent certainty, the best way to prevent tendinopathy is to look after your muscles and tendons by not over-exerting yourself, but keeping them strong and flexible by doing exercise. Warming up before exercise and cooling down afterwards by stretching your muscles is also recommended.
What is the treatment?
The treatment may depend on the kind of tendinopathy, but in most mild cases the RICE therapy is advised:
- Rest until the injury improves
- Ice – apply cold
- Compress the injury with a bandage or brace
- Elevate – keep the injured tendon raised while at rest.
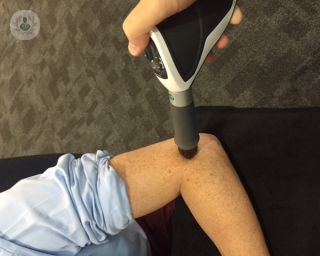
Painkillers may be prescribed to deal with the pain – particularly NSAIDs if there is inflammation. In more severe cases, shockwave therapy or surgery may be necessary.