How has the treatment of pelvic prolapse changed
Escrito por:Pelvic prolapse is when one or more of the organs in your pelvis (bowel, uterus, bladder) slip down into the vagina from their usual position. Symptoms can often be managed with lifestyle changes, but do sometimes require surgical treatment. Ms Renata Hutt, a leading obstetrician and gynaecologist, explains what pelvic prolapse is and what advancements have been made in treating it.
What is pelvic prolapse?
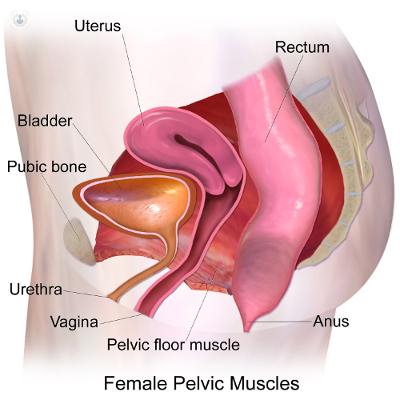
Pelvic organ prolapse refers to a herniation of the pelvic organs such as the uterus, the womb, bladder or the rectum through the vaginal walls. It is a common condition which affects many women. One in five women will develop symptoms from the weakening of the pelvic floor and one in ten of those will require surgery.
Pelvic floor organs are normally supported by the group of muscles and ligaments referred to as the pelvic floor. When they are weakened or stretched, women can experience symptoms of prolapse. Prolapse can be mild and may just involve a bulge through the vagina or sometimes the organs can completely protrude outside.
How can pelvic prolapse be managed and treated?
Mild prolapse will not usually require any treatment and women may not even be aware of it. Some women who have symptoms will need some treatment and its management and will depend on the severity of their problem.
There are simple measures women can take to improve the prolapse, such as lifestyle changes. These include losing weight, avoiding heavy lifting and avoiding constipation. These changes can quickly improve the symptoms of mild pelvic prolapse. Pelvic floor exercises can have a great impact and improve the pelvic floor muscles. Some women will need to try a combination of treatment options, which is they do not prove successful will require surgical intervention.
What advancements have been made recently in treating pelvic prolapse?
Traditionally, pelvic prolapse was treated using vaginal surgery, utilising surgical techniques such as sutures. Also, vaginal hysterectomy and anterior and posterior repair were the main treatment options chosen. They have a success rate of improving prolapse of 80 to 90% but long-term, using these techniques it became apparent that prolapse recurrence was a problem. To reduce the risk of recurrence and to retain the anatomical function of the vagina a number of new procedures were introduced which mainly made use of a mesh repair.
Meshes have traditionally been used in abdominal surgery for hernia repair and for such surgeries they have been used for a long time. The introduction of using meshes to treat pelvic prolapse is fairly recent. This type of treatment allows us to interlay the mesh material between the vaginal wall to strengthen the pelvic floor, thus retaining the anatomical structure of the vagina.
However, meshes in the vagina have been associated with more complications which became apparent very recently. Although many women will benefit from mesh treatment, there are complications, such as mesh erosion rates, infections and pain, which have been a problem for a number of women. Meshes therefore have been withdrawn from the treatment of pelvic prolapse and are not recommended unless they are for specific women with a high risk of recurrence or they are done by specialists who are trained to perform such surgeries.
Educating women with pelvic prolapse on the various treatment options and the potential risks and benefits of mesh repair is an important step in counselling such patients.
To improve the repairs performed on pelvic prolapse and to reduce the risk of any recurrence, there are a number of other procedures used such as laparoscopic surgery which can successfully treat and prevent pelvic prolapse.
These techniques are clearly advances in pelvic floor surgery which introduces the laparoscopic approach to the pelvic floor. These surgeries are done in specialist centers by trained individuals and many women may need to be referred to a specialist with this expertise.
If you would like to find out more, make an appointment with a specialist.


