Kавернома
What is a cavernoma?
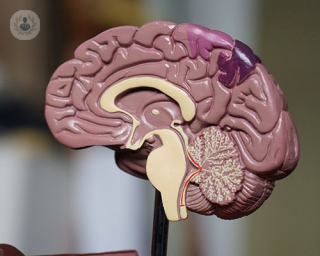
A cavernoma is a cluster of abnormal blood vessels, usually found in the brain and spinal cord. They are also known as cavernous angiomas, cavernous hemangiomas or cerebral cavernous malformation (CCM). A typical cavernoma looks like a raspberry and is filled with blood that flows slowly through vessels that are like caverns.
What are the symptoms?
Often a cavernoma doesn’t cause any symptoms but when symptoms do arise, they can include:
- Haemorrhage, when a blood vessel in the brain ruptures, causing bleeding
- Seizures
- Headaches
- Neurological problems like dizziness, balance problems, slurred speech and double vision
- Weakness
- Memory problems and problems concentrating
- Tiredness
- A type of stroke called a haemorrhagic stroke
Seek medical help immediately if you experience any of the aforementioned symptoms.
The severity of symptoms and duration of symptoms can vary, depending on the location of the cavernoma and the type. The cells lining the cavernoma are normally thinner than those of normal blood vessels which means that they are more prone to leaking. Severe bleeding or haemorrhages due to blood leaking can be life-threatening.
How is a cavernoma diagnosed?
Cavernomas are mostly diagnosed with an MRI scan that is being done for other neurological reasons. A detailed picture can be made of the brain and spine. Sometimes a contrast dye might be injected into a vein in your arm to get a better look at the blood vessels.
A CT scan or angiography can also be used, but are not as reliable as an MRI scan.
If there is a family history of the condition, genetic testing can be carried out to identify any changes associated with cavernomas in genes.
What causes a cavernoma?
For most cases, there is no clear reason as to why a cavernoma develops. Less than 50% of cases are thought to be genetic.
Some cases have been linked to radiation exposure, like having previously undergone radiotherapy on the brain.
Can a cavernoma be prevented?
There is nothing to prevent a cavernoma but genetic testing can be carried out to determine whether a person is at risk of developing a cavernoma. There is thought to be a 50% chance of a child developing a cavernoma if one parent has the genetic type of cavernoma.
How is a cavernoma treated?
Treatment will vary depending on the person, the size of the cavernoma and location. If there are no symptoms, your doctor might recommend monitoring the cavernoma with MRI scans on a regular basis to watch out for any changes in the malformation.
Symptoms such as headaches and seizures caused by the cavernoma can be managed with medication. More invasive treatments might be offered to reduce the risk of haemorrhages in the future. These treatments can include:
- Neurosurgery: under general anaesthetic, the cavernoma is removed
- Stereotactic radiosurgery: a concentrated dose of radiation is aimed directly at the cavernoma so that it becomes thickened and scarred. This treatment is usually only carried out if the cavernoma is too difficult to remove with neurosurgery.
What specialist would I see?
A neurologist or cerebrovascular neurologist, trained in the brain and nervous system will treat a cavernoma.