Atrial fibrillation: What are the signs and symptoms?
Escrito por:In this informative guide, highly respected consultant cardiologist and electrophysiologist Dr Shui Hao Chin shares his expert insight on the key warning signs of atrial fibrillation and how the condition is diagnosed. The revered specialist also details how atrial fibrillation can affect the heart’s function over time and reveals the most common approaches to treatment.
What is atrial fibrillation?
Atrial fibrillation is an abnormal heart rhythm characterised by fast, disorganised activation of the upper chambers of the heart, known as the atrium. It is caused by extra electrical signals firing within the atrium from many sites simultaneously. This type of heart rhythm can be intermittent or continuous in occurrence.
For atrial fibrillation that occurs intermittently, we generally accept a cut-off of thirty seconds or more before a diagnosis of atrial fibrillation is made. This is in contrast to the non-sustained extra heartbeats that can occur in the atrium.
What are the symptoms of atrial fibrillation?
Most patients with symptomatic atrial fibrillation experience palpitations in the form of feeling the heartbeat running fast and irregularly. Others complain of breathlessness, chest tightness and fatigue during atrial fibrillation.
For some patients, episodes of atrial fibrillation classically occur at night, leading to disturbed sleep. In extreme cases, some patients experience dizziness or near or complete blackout during episodes of atrial fibrillation.
Unfortunately, some patients may not experience any symptoms with atrial fibrillation. One of the major devasting sequalae of atrial fibrillation is stroke. Atrial fibrillation accounts for twenty to thirty per cent of stroke caused by blood clots arising from other parts of the body, known as thromboembolic stroke. It also accounts for ten per cent of stroke with unidentified cause, known as cryptogenic stroke. It is only when these patients experience a stroke that the diagnosis of atrial fibrillation is made.
Other patients experience breathlessness, fatigue and reduced exercise tolerance after being diagnosed with heart failure. Heart failure is essentially weakness of the pumping chamber of the heart and in the context of atrial fibrillation, this is driven by prolonged periods of a fast heartbeat and irregularity of the heart rhythm leading to uncoordinated contractile function of the heart.
How is atrial fibrillation diagnosed?
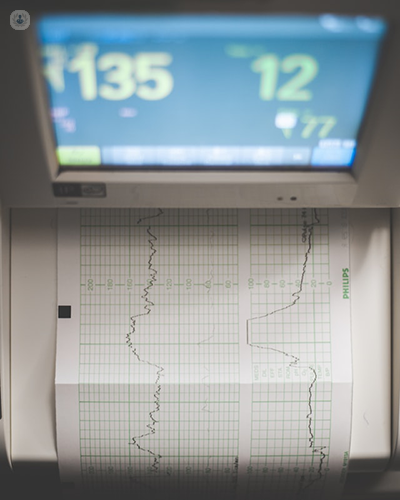
Objective evidence of atrial fibrillation is traditionally obtained on a heart tracing known as a 12-lead ECG, manifesting as irregular heart rate and an absence of distinct repetitive atrial activation (known as P-waves). In some cases, other evidence on the ECG of atrial fibrillation is visibly irregular waveforms known as the fibrillation waves.
It should be pointed out that in order to diagnose atrial fibrillation, a full 12-lead ECG is not required and a single ECG monitor with reasonable quality recording can also effectively establish the diagnosis. From the patient’s perspective, the patient may suspect atrial fibrillation through indirect evidence such as palpation of their own irregular pulse through pulse taking, warnings from home automated blood pressure monitors or smart watches. Nowadays, with the advent of wearable technology, atrial fibrillation can be diagnosed through smart watches and smart phone apps capable of ECG recordings, prompting subsequent confirmatory tests like a 12-lead ECG or a Holter.
What are the risk factors for atrial fibrillation?
Risk factors for atrial fibrillation can be divided into two categories. The first category is non-modifiable risk factors. These include increasing age, male sex, Caucasian ethnicity and lower socioeconomic status.
The second category is modifiable risk factors. These could be in the form of health-related behaviours and lifestyle, including excessive alcohol intake, tobacco use, caffeine consumption, vigorous exercise at the level of competitive or athlete-level endurance sports. Other modifiable risk factors include health factors and diseases, including elevated blood pressure, diabetes mellitus, elevated cholesterol, obesity, kidney diseases, sleep apnoea and chronic lung diseases like COPD.
What are the treatment options for atrial fibrillation?
Management of atrial fibrillation requires an integrated and multifaceted approach. First and foremost, the stroke risk of patients diagnosed with atrial fibrillation should be assessed. Using robustly validated risk calculation, we can identify patients suitable for blood thinners, known as anticoagulants, to reduce their stroke risk significantly. Those who are at low risk of stroke are not required to take an anticoagulant by the guidelines, nor aspirin in the context of atrial fibrillation.
The second aim of management of atrial fibrillation is the control of the associated symptoms. In patients with atrial fibrillation and a fast heart rate, a beta blocker is typically prescribed to help to slow the heart rate. This can be prescribed by a GP. However, beyond that, atrial fibrillation can be managed with more specialised antiarrhythmic drugs, prescribed by cardiologists.
Patients with persistent atrial fibrillation may be treated with DC (direct current) cardioversion, a procedure which involves delivering electrical shock to the heart through external pads to reset the heart rhythm. Prior to cardioversion, these patients will be mandated to take an anticoagulant for a period of time.
Modern treatment of atrial fibrillation is heralded by a procedure known as catheter ablation. This is commonly done as a day case procedure, sometimes involving an overnight stay. The procedure can be done either under sedatives or general anaesthesia. It involves passing wires and catheters up from the top of the legs through the vein into the heart, making a small hole to cross from the right to the left upper chamber of the heart. Once in the top left upper chamber of the heart, ablation is performed to cauterise the area of the heart responsible for erratic electrical firing that causes atrial fibrillation. The ablation procedure itself is safe and normally carries an overall procedural risk of up to one per cent.
If you are concerned about the symptoms of atrial fibrillation and wish to schedule a consultation with Dr Chin, you can do so by visiting his Top Doctors profile.


