Glaucoma and ocular surface disease - a dangerous combination! – Part 2
Autore:Ocular surface disease can be a big problem for glaucoma patients – even to the point where they may stop taking their glaucoma medication (see part 1 of this article). Is there a solution to this problem? Leading ophthalmologist Mr Shabbir Mohamed talks treatments and the future.
What can be done to combat ocular surface disease in glaucoma patients?
The first step is to appreciate the importance of understanding the problem and how it can impact the quality of life of glaucoma patients. We have found that it is essential to control intraocular pressure but also to look after the health of the ocular surface at each visit when managing patients with glaucoma for good long term outcomes.
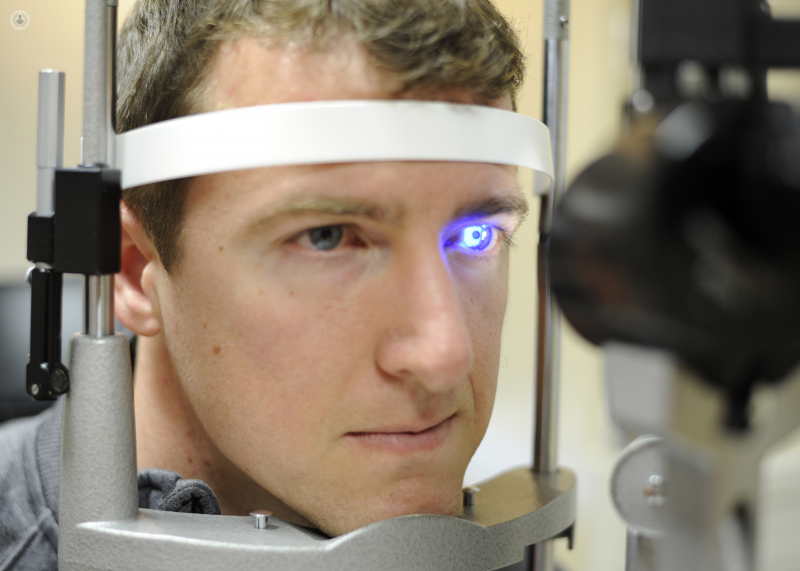
It is essential to systematically evaluate the patient and their ocular surface to enable recognition of moderate to severe OSD and take active intervention to halt the inflammation and scarring that accompanies this. Unfortunately, there is no single test available that can identify worsening OSD and this evaluation is based on the expertise of the ophthalmologist.
If OSD is present, the ocular surface can be supported by a variety of means, ranging from lubrication to use of preservative-free glaucoma medication and in some cases systemic treatments. This all takes time and requires continuity of care, which is unfortunately becoming a difficult thing to achieve in modern healthcare systems.
What are the benefits of managing patients in this way?
There is good evidence that treating OSD in the general population improves quality of life significantly. This is therefore the first benefit.
In addition, we have found that improving the ocular surface in glaucoma patients helps to lower intraocular pressure and also helps to keep it low over the longer term in some patients. We published a paper in the Journal of Glaucoma on this phenomenon which we called ‘Ocular Surface Disease exacerbated glaucoma’. We postulated that this may be because the final outflow pathway of the intraocular fluid is via the ocular surface and by improving the health of the ocular surface and reducing inflammation, we are probably helping to reduce the resistance to the outflow and thereby reducing intraocular pressure. This is a hypothesis at this stage and needs more research to look at in more detail.
The third benefit of this approach is that if the patient requires surgery, the outcomes are likely to be better as the ocular surface is less inflamed and less prone to scarring, which is the process by which glaucoma surgery fails. Anecdotally, we have observed this and we advocate ocular surface optimisation prior to glaucoma filtration surgery.
Perhaps the most important benefit of this approach is that the doctor-patient relationship is maintained and improved. This leads to greater trust in the healthcare system which is of great benefit to society. The effect on the clinician is possibly greater than that on the patient.
Hopes for the future
It is encouraging that most glaucoma drops are now available in a preservative-free form. This is a good development, especially for those patients at high risk of developing moderate to severe OSD-related problems in their lifetime. Pharmaceutical companies are also more aware to assess the ocular surface effects of newer medications before release to the general public.
There are also developments in tools to identify patients who are developing worsening OSD, which may reduce reliance on expertise which is difficult to achieve in this area. This would enable earlier interventions to reduce the disease burden in this group of patients.
We are developing alternative approaches to control intraocular pressure other than multiple drops, which are less invasive than our traditional surgical methods. This may translate to lower morbidity for our patients in the longer term.
In my working life, I have seen valuable developments in this area of treatment and see less of the severe end of ocular surface problems in glaucoma patients. This gives great hope for the future.