A detailed explanation of thulium laser resection: part 2
Escrito por:In the second article of a two-part series, leading consultant urological surgeon Mr Ahmed Ali further explores thulium laser resection, discussing the specific techniques utilised and how this method can reduce complications.
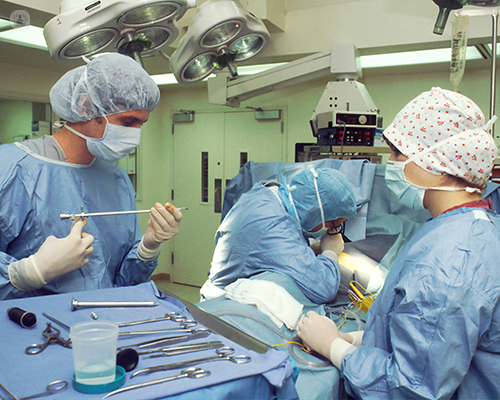
Can you explain the procedure in depth? What specific techniques or tools are utilised and how do they contribute to improving patient health?
The use of laser allows us to perform the procedure with a general anaesthetic or with spinal anaesthesia, meaning that we're not limited to general anaesthesia because of the risk of an obturator jerk. This is extremely useful, particularly in patients who have respiratory issues where they cannot have general anaesthesia. It shortens the procedure time and therefore shortens the anaesthesia time. The shorter the operation is, the more beneficial it is to the patient.
Furthermore, it's very useful in patients who are on anticoagulation because the risk of bleeding is very low. Postoperative recovery and rapid return to normal activities are much quicker with the laser compared to the diathermy.
There are multiple aspects that this procedure helps us with. In our practice, we use the Rocamed SAM thulium laser. I use the setting of two joules and 10 hertz. We use 20 watts of energy and we use a 550 micron thulium laser fibre to perform the procedure. We use a resectoscope, which provides continuous irrigation for better visibility and we use a stabilising laser access sheet to ensure that the laser fibre remains in vision all the time.
How does thulium laser resection contribute to reducing complications like bleeding, perforation, or stretcher formation compared to other resection methods?
The thulium laser is a brilliant hemostatic-powered laser and lasers, in general, are very precise in the nature of resection. The power of such lasers aids us to reduce the risk of perforation and reduce the risk of bleeding. The use of laser provides an extremely controlled forward movement, so the risk of deep resection is also limited, therefore this enables us to give most of those patients post-operative chemotherapy, reducing their risk of recurrence.
For patients on anticoagulation, we generally restart their anticoagulation in a shorter period of time compared to the old technique, with the diathermy, when we used to keep them off anticoagulation for two weeks, to reduce the risk of post-operative bleeding. With using the laser, we now restart their medication within 48 hours.
The risk of catheterisation is lower and most patients that we have performed the procedure on have left the hospital without a catheter, as a day case procedure. Our initial experience showed that those patients are less likely to suffer from irritative symptoms; they do not experience the usual frequency and urgency to pass urine after the operation. This therefore reduces either their hospital return visits or their visits to the general practice, which were previously quite high in patients with bladder cancer who recently had an operation.
To date, our initial experience has been positive. We are currently in the prospect of collecting all this data and we have been invited to participate in an international study now, which will validate the use of laser and bladder cancer.
In terms of long-term oncological outcomes, what insights can you share regarding the recurrence rates of overall cancer control achieved using the thulium laser recession for bladder tumours and how does this approach fit within the broader spectrum of bladder cancer management?
The laser itself is very new, therefore we do not currently have long-term data for oncological outcomes such as the risk of recurrence or progression. However, the technique of en bloc has been described in some studies to have better recurrence rates than the conventional transurethral resection of bladder tumours (TRBT) and reduces the risk of seeding, but there are no randomised controlled studies that have shown there is an added benefit for either laser use or en bloc resection.
That being said, we have found that there are two main advantages for using the laser; one is it provides better specimen analysis for the pathologist and reduces the need for return to the theatre either for resection or for control of bleeding. It also reduces the risk of bladder perforation and improves our ability to administer postoperative mitomycin chemotherapy.
If you are considering thulium laser resection and would like to book a consultation with Mr Ali, do not hesitate to do so by visiting his Top Doctors profile today


