Painful clicking of the knee and solutions explained
Escrito por:Mr Graeme Nicholas Fernandez, one of the UK’s most experienced orthopaedic surgeons, provides you with a list of conditions that could be causing painful knee clicking and the treatment available for these conditions. He also clarifies how you can receive help during the coronavirus crisis.
Is clicking of the knee normal?
No, painful clicking of the knee is not normal and warrants medical attention.
What conditions can cause painful clicking?
- Damage to the meniscus (e.g. a torn meniscus) from a sporting injury or simply squatting down
- A spontaneous degenerative meniscal tear
- Loose bodies (pieces of cartilage or bone) in the knee. As well as painful clicking, they can cause the knee to jam momentarily – this is known as locking
- Damage to the joint’s surface (e.g. osteochondritis dissecans)
- Arthritis of the knee
- Inflammation of the surrounding soft tissues (ligaments, tendons and bursa)
- Pain from the hip – pain from hip arthritis can sometimes be felt in the knee
When should someone see a doctor/specialist for painful knee clicking?
This depends on the severity of the pain:
- Clicking but no pain: This can be safely ignored for around six weeks. If there is no improvement, consulting a physiotherapist might be helpful.
- Mild pain: This pain should be addressed by a physiotherapist.
- Severe pain: This warrants seeing a doctor within a few weeks. If your mobility is very restricted go to see your doctor as soon as you can.
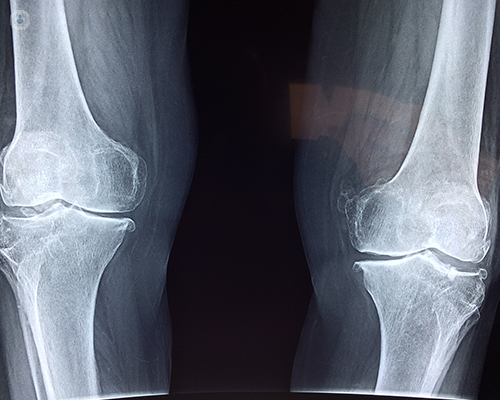
Diagnosis
The diagnosis is made by assessing the patient clinically and possibly with x-rays and an MRI (magnetic resonance imaging) scan. Most patients will need to see a physiotherapist first, as well as trying rest and anti-inflammatory medication. If symptoms are severe, an appointment with an orthopaedic surgeon should be arranged.
How is the painful knee clicking treated?
Treatment depends on the diagnosis:
Damage to the meniscus and meniscal tears
This may require keyhole surgery to repair or trim the damaged meniscus, providing there is no significant arthritis in the joint. If the pain is mild it is worth waiting a few months as the pain may settle without surgery.
Loose bodies (pieces of cartilage or bone)
These almost always require removal as they can cause significant damage to the joints. This is usually done via keyhole surgery.
Osteochondritis dissecans
This may require keyhole surgery to trim or stabilise the loose fragment, or it may need removing.
Arthritis of the knee
This is treated initially with activity modification
- The patient is advised to stop activities that make it worse
- Weight loss if appropriate
- Physiotherapy
- Anti-inflammatory medication
- Non-weight bearing exercises (e.g. cycling, swimming, rowing) to help strengthen muscles and stabilise the knee
Injections of steroids into the knee may give short-medium term relief. A small proportion of patients benefit from viscosupplementation injection into the knee.
An off-loading knee brace may be helpful if just one side of the knee is worn
Surgery is reserved for severe symptoms.
Younger patients with joint deformity may be offered an osteotomy to correct the deformity. This can delay joint replacement for many years. Joint replacement of one, two or all three compartments of the knee is very effective at reducing pain and improving function. It is possible to play golf and tennis and some patients return to skiing. Recovery from surgery is long with benefits continuing over 18 months. Complying with physiotherapy instructions is very important. It should be born in mind that four out of five patients are very happy with their knee replacement but one out of five is not.
During the current COVID-19 pandemic joint replacement has been halted as the mortality rate is higher if the patient develops COVID-19 in the first 6 weeks after surgery. Joint replacements currently are reserved for patients with the most severe pain and who are struggling to walk but are otherwise fit. As the pandemic passes, surgery will again be offered to all patients.
Inflammation of the surrounding soft tissues (ligaments, tendons and bursa)
Bursitis and tendonitis rarely need surgery. They usually respond to rest, anti-inflammatories, application of ice pack, anti-inflammatory gel and physiotherapy. Occasionally, steroid injections may be indicated.
Pain from the hip
Certain hip conditions cause pain only in the knee, such as osteoarthritis of the hip. A diagnostic injection into the hip will usually relieve the knee pain in the short term. Hip replacement may subsequently be needed
What habits should people with painful knee clicking avoid
Any activity that makes it worse should be avoided. It’s especially important to avoid applying high loads to the knee e.g. by running on hard surfaces or carrying heavy weights.
How to see an orthopaedic surgeon during the COVID-19 crisis
Some surgeons are offering video consultations. Face-face consultations for non-urgent patients are currently not being performed but will be resumed probably within a month or two
You can request a consultation with an orthopaedic surgeon through a general practitioner, or if you wish to be seen privately, contact your chosen consultant’s secretary. If you have health insurance, contact them directly, or contact your private hospital to request an appointment.
Mr Fernandez is one of the most experienced orthopaedic surgeons in the UK. Click here to learn how he can help you and to arrange an online or face-to-face consultation.


