What is neutropenia?
Autore:Having a low blood count can put you at an increased risk to certain problems, and when your white blood cell count is low, you are more prone to contracting infections. In fact, sometimes it is repeated infections that send people to the doctor initially, before being diagnosed with an abnormal blood count. One such type of blood count is a neutrophil count, but what are neutrophils? Dr Jonathan Sive, a top haematologist, explains what they are and what a low neutrophil count can mean for your health.
What is neutropenia?
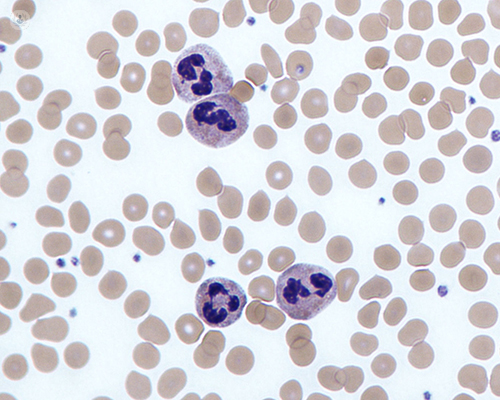
Neutrophils are one of the main types of white blood cells and they are important for protecting the body against bacterial infection. Neutrophil numbers are counted as a part of a standard full blood count (FBC), and should normally be in the range of 2.0-7.0 x 109/L, although specific normal ranges may vary slightly between hospital laboratories. Neutropenia is a neutrophil count which is reduced below this range.
Neutropenia can be divided into mild, moderate and severe, based on the count:
- Mild = 1.0-1.5 x109/L
- Moderate = 0.5-0.9 x109/L
- Severe = <0.5 x109/L
What are the symptoms of neutropenia?
Neutropenia is often an incidental finding which does not cause any symptoms. If neutropenia is moderate or severe it can put people at an increased risk of infection, which may well be the problem they initially go to the doctor with. This can vary from a mild infection that is managed by a GP, or a more serious infection that leads to hospital admission.
What are the possible causes of neutropenia?
Neutropenia can be a racial-variant: African and African-Caribbean people often have a low neutrophil count, which is normal. Some drugs can cause neutropenia, as can viral infections, some auto-immune conditions and occasionally vitamin deficiencies. In some cases, neutropenia may be due to a problem in the bone marrow, and if it is persistent without an obvious explanation, then review by a haematologist is recommended.
What investigations are required?
Standard investigations can usually be done with blood tests from the clinic. Occasionally, a bone marrow biopsy is required – this involves taking a small sample from inside the bone at the top of the hip. This is a day-case procedure that is done under local anaesthetic and it allows more detailed tests to be done on the maturing blood cells.
What treatment may be required?
In many cases, no specific treatment is required, apart from regular monitoring, and prompt antibiotics for any infections. If the neutrophil count is persistently very low, then sometimes preventative antibiotics and antiviral medications may be recommended to reduce the risk of infection. Growth factor injections are also occasionally used to increase the neutrophil count. Specific treatment for a bone marrow problem depends on the nature of the condition and should be managed by a haematologist.
Dr Jonathan Sive works at the renowned UCLH Macmillan Cancer Centre in London where he treats patients with blood disorders, blood cancer and abnormal blood counts.


