What causes retinal detachment?
Written by:Retinal detachment is a potentially devastating, sight-destroying eye condition. If not treated quickly, it can cause permanent loss of sight. What causes this debilitating condition? Top ophthalmologist Praveen Patel explains:
The retina
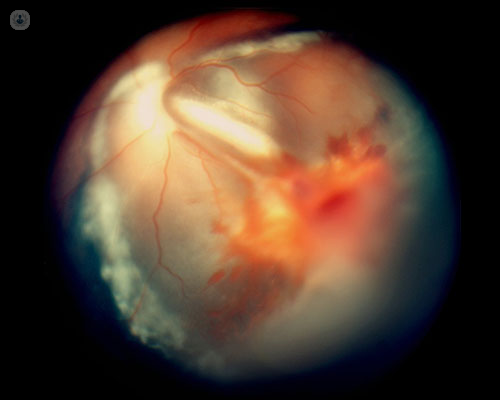
The retina is a layer of light-sensitive cells found on the back wall of the eye. The cone and rod light-detecting cells found here convert light that enters the eye into electrical signals, which are sent to the brain to be interpreted as vision. This means that the retina is essential for our ability to see.
Unfortunately, the retina can peel away from the back of the eye, cutting it off from its blood supply. Without oxygen or nutrients delivered by the blood, the light-sensitive cells of the retina will cease to function, and loss of sight follows.
Causes of retinal detachment
Detached retinas occur in one of three ways:
- Rhegmatogenous retinal detachment – a tear or break appears in the retina, perhaps due to traction from separation and liquefaction of the gel-like vitreous or injury to the eye. The retinal tear lets fluid get under the retina, weakening its attachment to the RPE (retinal pigment epithelium) layer of cells below, before the two layers separate completely. This is the most common type of retinal detachment.
- Tractional retinal detachment – less common than rhegmatogenous detachment, here the retina is pulled away from the RPE by scar tissue on the surface of the retina contracting. This can be seen in conditions such as severe diabetes.
- Exudative retinal detachment – other retinal diseases, e.g. inflammatory disorders, or trauma to the eye causes fluid to leak between the retina and RPE without causing a retinal tear.

Risk factors
People of any age can get a detached retina, but the risk becomes greater the older you get. Other risk factors apart from age include:
- Short-sightedness (myopia)
- Eye injury
- If you have had an eye operation, like cataract surgery
- Other eye diseases/disorders
- Other disorders, such as diabetes
- A family history of retinal detachment
What to watch out for: symptoms of a detached retina
The two key signs of a detached retina are seeing flashes of light in your eye, and an increase of floaters (those little shapes or ‘cobwebs’) in your field of vision, particularly if they appear in a sudden shower. If you experience these symptoms, you should consult an eye health care specialist ideally within 24 hours, before the condition progresses. If it is allowed to progress, more serious symptoms can follow, including:
- A dark curtain or shadow moving across your field of vision
- A dense shadow in the peripheral vision which slowly progresses towards central vision
- Straight lines appearing curved
- Central vision loss
Any loss of vision is a medical emergency, and you should consult a doctor as soon as possible.


