So, the big day is here! After nine long months, your baby is finally making its way into the world. The life you have created is ready to truly begin. As you hold your tiny, new human in your arms for the first time, so many thoughts rush through your head. Is this real? How did we make something so perfect? This is the happiest day of our lives. The cord is cut. It is time for the little one to join the family. One thing that probably doesn’t cross your mind is what happens to the umbilical cord. It’s done its job. Probably just goes in the bin, right? Believe it or not, even after sustaining a life for nine months, umbilical cord blood still hides a potentially life-saving secret…
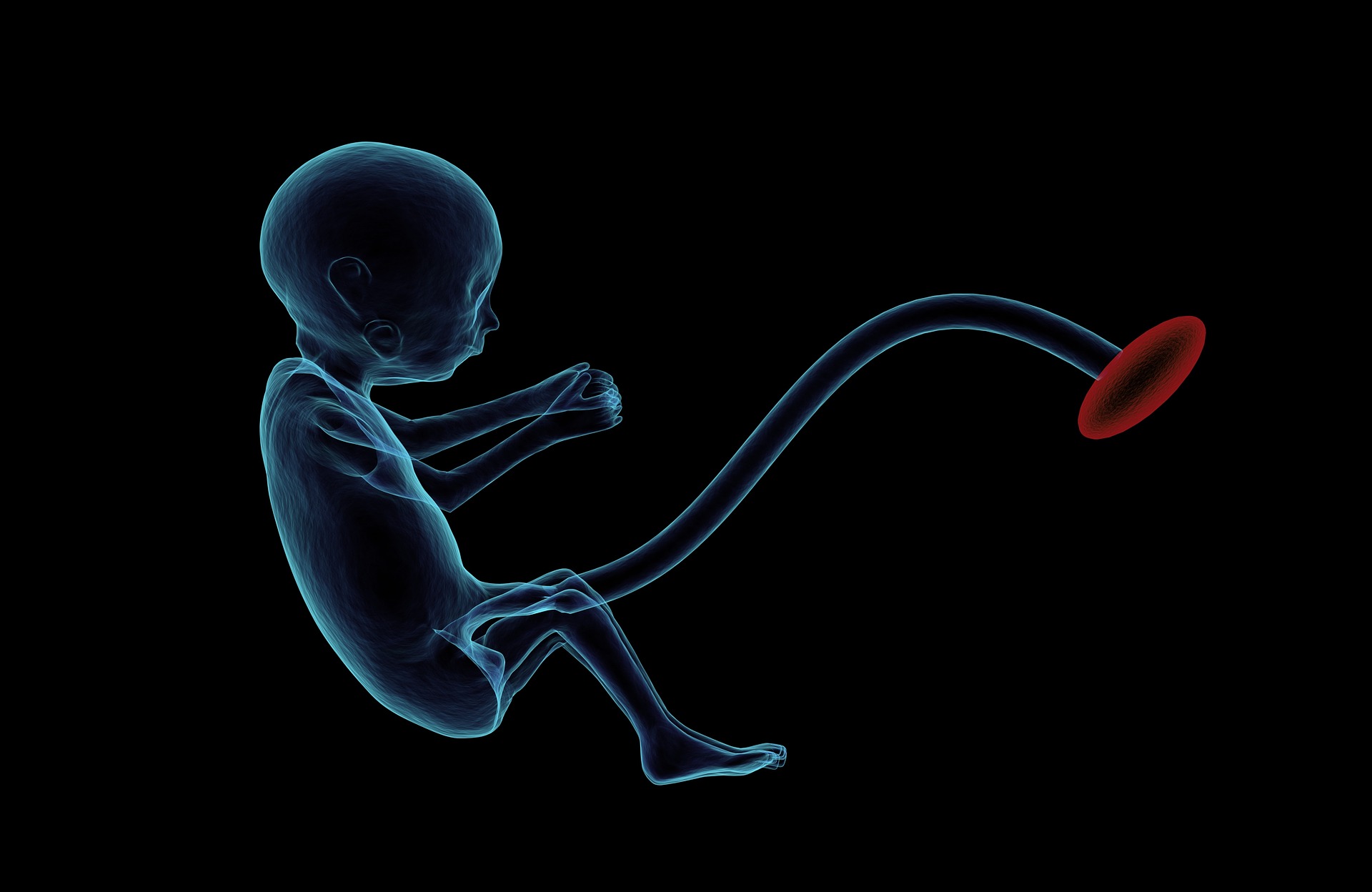
Stem cells. A somewhat controversial topic. Despite the association with human embryos, it turns out that one of many places they are found is in the umbilical cord (specifically the cord blood), which so often is thrown out in the hospital rubbish. Saving these otherwise unwanted cells could potentially save a leukaemia patient’s life.
So, what exactly are stem cells and how do they work? How can the umbilical cord blood save a cancer patient?
What are stem cells?
Since it was discovered that they could hold the key to curing many of the worst diseases that affect humanity, stem cells have been mired with controversy. Not least because they are most famously found in human embryos. While the harvesting of stem cells from petri-dish blastocysts raises ethical questions, the debate has thrown up a lot of misinformation about what stem cells actually are. Let’s set the record straight.
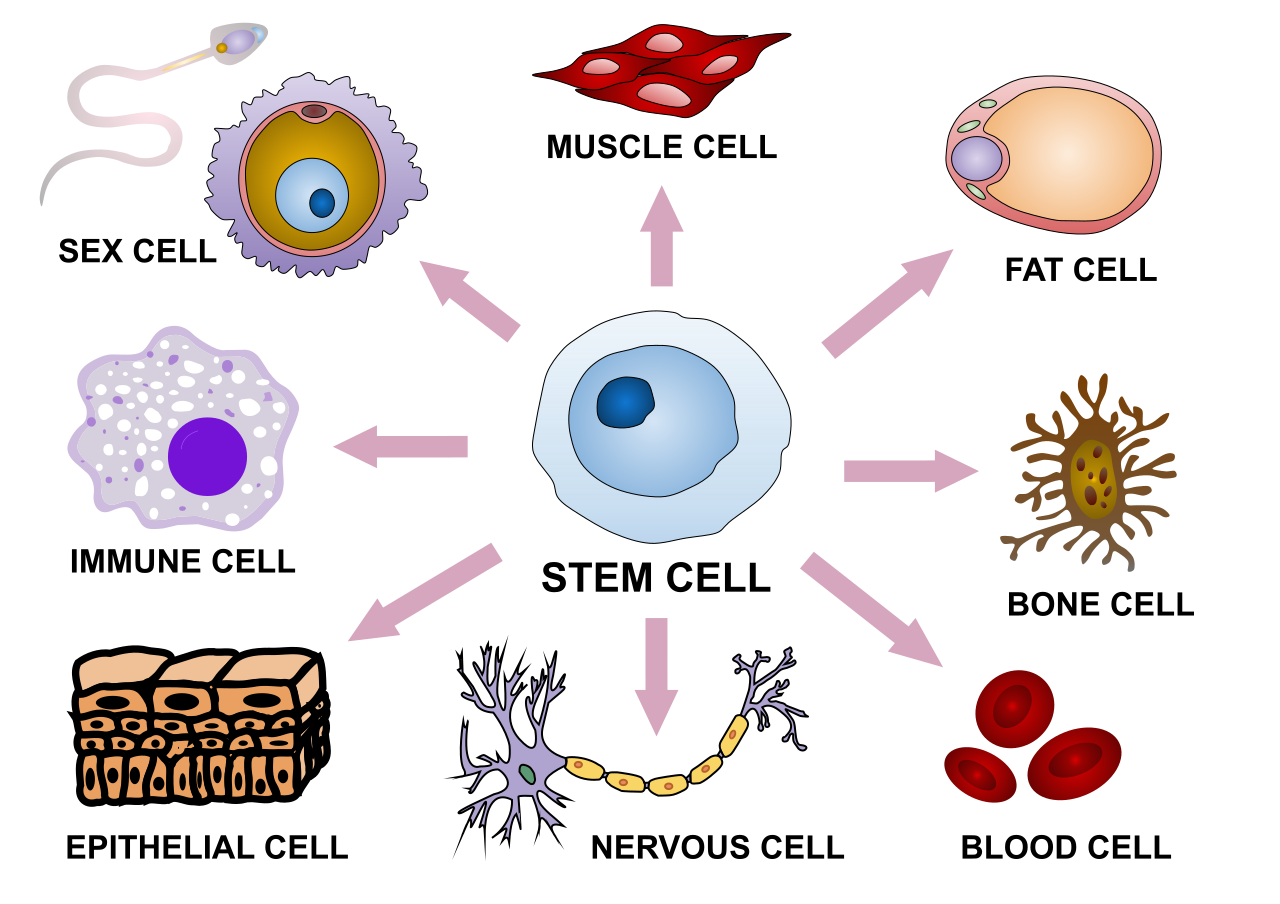
Most of the body’s cells have a specific form and function. Liver cells are completely different from brain cells. Nerve cells are specialised to transmit electrical impulses to and from the brain, while red blood cells are packed with haemoglobin to allow them to carry oxygen.
Stem cells are a kind of “blank slate” – a special kind of basic cell that have the potential to turn into almost any other kind of cell in the body. This process is called differentiation.
While most cells in the body have a limit on the number of times they can divide and replicate before they break down, stem cells can divide seemingly limitlessly. Every time they divide, each copy can either remain a stem cell or differentiate into a more specialised cell type.
There are several types of stem cells:
- Embryonic stem cells – found in human embryos. They are pluripotent, which means they can differentiate into virtually any kind of cell.
- Adult stem cells – also termed “non-embryonic stem cells”, these are found in developed organs and tissues in the body, including the blood. The name is misleading, as they are found in children and infants as well as adults. They can generally only differentiate into a certain range of cells, depending on where they are found.
- Induced pluripotent stem cells (iPSCs) – adult stem cells that have been genetically reprogrammed to respond like embryonic stem cells, theoretically giving them the ability to differentiate into any cell that an organ or tissue needs. Research is ongoing into producing these safely.
- Cord blood stem cells and amniotic fluid stem cells – similar to adult stem cells, but found in the womb, in the umbilical cord and amniotic fluid, respectively.
Why are stem cells important?
There is a lot of interest in stem cells due to their potential in replacing and regenerating damaged tissue. Researchers around the world are developing ways to better control how stems cells differentiate and conducting clinical trials to see if stem cell treatments could prove a solution for various diseases. Possible applications for stem cells include neurodegenerative conditions, such as Alzheimer’s, Parkinson’s, and multiple sclerosis, heart disease, and even HIV/AIDS. Stem cells could revolutionise the world of medicine in the future. However, research is one thing and successfully treating the masses is another.
There is one type of stem cell treatment which has proved effective. Indeed, it has been an accepted and widely used treatment for over 30 years. This involves a transplant of haematopoietic stem cells (HSCs).
Haematopoietic stem cells: bone marrow and cord blood
HSCs are a type of adult stem cell. They can differentiate into any type of blood cell, from the oxygen-carrying red blood cell (RBC) to the various white blood cells that form part of the immune system and combat infection. They can also become platelets, involved in the blood-clotting process. HSCs are found in the bone marrow, a spongy tissue inside bones, where blood is created.
Bone marrow transplants have been used for decades for treating various types of blood disorders, cancers, and immune diseases. The HSCs in the transplanted bone marrow are the key. First, the patient’s own defective immune system and HSCs are destroyed using chemotherapy or radiotherapy, and are replaced by healthy transplanted ones.
Diseases that respond to treatment with haematopoietic stem cells transplants include:
- Blood cancers, e.g. leukaemia, lymphoma
- Blood disorders, e.g. sickle cell anaemia, thalassaemia
- Bone marrow failure – this is when the bone marrow doesn’t function properly, not producing cells correctly.
- Immune system disorders – i.e. the immune system doesn’t work properly.
- Metabolic disorders – waste products are not broken down properly in the body.
Bone marrow transplants do come with certain drawbacks. Harvesting the stem cells from the donor is done under general anaesthetic, but the area where the needle was inserted into the bone can be painful after the procedure. There are also general risks associated with minor operations.
This is not the case with umbilical cord blood. Cord blood contains higher levels of HSCs than normal blood, and they have the same properties as those found in bone marrow. The difference is that you don’t need an invasive procedure to get these stem cells. The umbilical cord is usually just thrown away after birth – with the stem cells it contains in tow! By saving the cord blood, we have a supply of HCSs without having to find a donor.
Cord blood stem cells – pros and cons
Cord blood isn’t a new idea – it has been used to treat certain blood diseases in children since 1989. The haematopoietic stem cells it contains work much the same way as those in bone marrow. They can produce every kind of blood cell and can be used to treat the same conditions.
Advantages of cord blood stem cells include:
- Easy supply of HCSs, without needing to harvest another person’s marrow
- No risk to baby or mother (they are already finished with the cord!)
- Lower risk of graft-versus-host disease than in bone marrow transplants
There are some reports that cord blood may contain other stem cells besides HCSs, which may be able to differentiate into other kinds of cells. However, this is not widely accepted at present. More research needs to be done, and is indeed underway. There may be more benefits of umbilical cord blood waiting to be discovered.
There are, however, a few disadvantages:
- While cord blood has more HCSs than normal blood, it has a lower concentration than in bone marrow. This means adult patients may need two volumes of cord blood, which means more donations are needed per patient.
- Supply is dependent on donations.
Cord blood banking
One of the biggest problems with using umbilical cord blood stem cells is that the majority of them are simply thrown away. After most births, the placenta and umbilical cord are disposed of, as per hospital practices. The parents must give permission, and in some cases, make arrangements for the cord blood to be taken and stored for medical use. This simple gesture could save a life.
This is complicated by the fact that there are various private cord blood banking services. Many of these push the idea that parents should pay to bank the stem cells in case their own child needs them in the future. While the child should be an exact genetic match for the stem cells, it is highly unlikely that they will ever need them, meaning that most private donations will never be used.
Donating cord blood to a public blood bank, on the other hand, increases the supply available to people who need it. Many doctors support this action. Also, the more donations of cord blood, the more chance a patient with leukaemia or lymphoma will be able to find a matching donor to get a compatible transplant.
Cord blood: in conclusion
Stem cells obtained with no harm done to anyone, no ethical quandaries, no cost to yourself. There you go now. Leaving the hospital for the first time with your newborn, cord blood safely banked. One life just beginning; another life, somewhere, at some point in the future, saved.

Sources:
https://www.nhsbt.nhs.uk/cord-blood-bank/what-is-cord-blood/
https://www.eurostemcell.org/cord-blood-stem-cells-current-uses-and-future-challenges
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3753204/
https://www.nhs.uk/conditions/stem-cell-transplant/what-happens/
https://www.healthline.com/health/stem-cell-research#types
https://www.stanfordchildrens.org/en/topic/default?id=what-are-stem-cells-160-38







Join the discussion