Appendicitis symptoms, causes and prevention
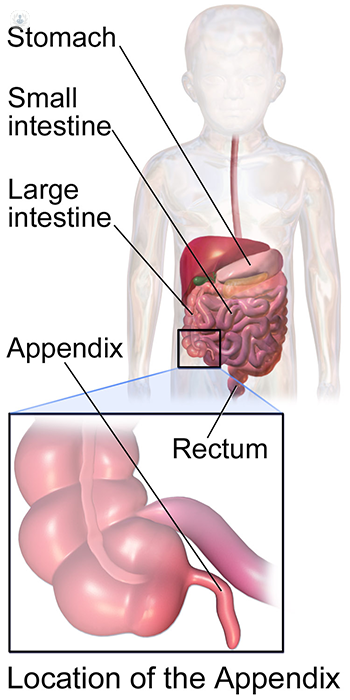
Autore:The appendix is a very small pouch that is attached to the large bowel, however, nobody knows what its exact purpose is. We do, however, know that removing the appendix is not harmful. Sometimes the appendix can become inflamed, which requires urgent medical attention. This is known as appendicitis. Mr James Kirkby-Bott, an experienced general surgeon, provides us with a summary of this condition, which is one to be aware of.

What is appendicitis?
Appendicitis is inflammation of the appendix. The appendix is a narrow tube of bowel that comes off of the caecum, which is the first part of the large bowel. You do not need it and it is thought to be due to an evolutionary process of the shrinking size of the caecum. It is about 6cm long and can lie in a variety of positions, but its base is always attached to the caecum with a clinical anatomical landmark called McBurney’s point. This can be found about 1/3 of the way from your belly button to the bony prominence that you can feel on your side, which is the front of the top of your pelvis.
The symptoms typically come on over the course of 12-24 hours. It can be serious and, if left untreated, the appendix can perforate. As a rough, but general, rule the sooner treatment commences, either in the form of antibiotics and/or surgery, the less severe the condition becomes.
Symptoms of appendicitis
The symptoms are similar in every age group. Symptoms progress in a stepwise pattern as listed in order here. However, we are all a bit different and different elements of the symptoms can present differently in some. Nevertheless, the vast majority generally follow the listed course:
- They start with feeling queasy and a vague discomfort throughout the abdomen.
- The queasiness can develop into nausea and vomiting and usually puts you off eating food. Eating food despite this can make the symptoms worse.
- As the inflammation of the appendix progresses, the general discomfort becomes a more profound pain felt in the lower half of the abdomen on the right-hand side.
- It can become painful to move and eventually you may prefer to lie still.
- It can cause a mild rise in temperature, but it is unusual for it to go above 37.5-38 degrees Celsius.
- The heart rate can rise.
- It can make you feel the need to empty your bowel and bladder more often and sometimes cause diarrhoea.
What causes appendicitis?
Good question, but there is no real answer! There are thought to be a variety of causes. Generally, however, the underlying cause results in an obstruction of the outflow of the appendix so it becomes blocked. The continued secretions then accumulate and increase the pressure in the appendix. This leads to inflammation. This, in turn, increases the pressure on the wall of the appendix, reducing its blood flow so it becomes ischaemic, more inflamed and, eventually, gangrenous and perforated. This sequence of events has many possible causes:
- It can be due to a hardening of a small amount of faeces getting caught in the appendix lumen called a faecolith.
- It can be due to intestinal worms (rare in adults).
- It can be due to a tumour causing blockage of the appendix (rare).
- It could be due to inflammation as a result of a virus (unproven but thought to be a common cause).
Read more: Appendicitis in children
Who is at risk of appendicitis and can it be prevented?
Everyone. It affects all age groups in equal proportion and men and women in equal proportion. The lifetime risk of developing appendicitis is about 13%. It doesn’t run in families, but as 1 in 10 people get appendicitis, it is common for several family members to develop this condition. There is no good evidence that diet influences the outcome or likelihood of developing appendicitis. There is also nothing you can do to reduce your own personal risk of developing appendicitis. However, as we get older, other conditions can mimic appendicitis, such as diverticulitis, which is inflammation of a diverticulum of the large bowel. The risk of developing diverticulum of the large bowel (known as diverticular disease) can be reduced by having a well-balanced diet that is high in fibre, from childhood.


