Diverticulitis
Dr Patrick Wilson - Gastroenterology
Created on: 11-05-2015
Updated on: 05-23-2023
Edited by: Conor Dunworth
What is diverticulitis?
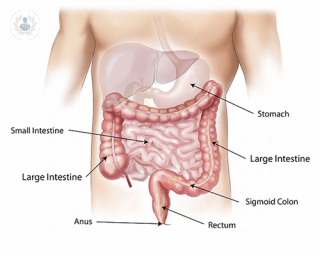
Diverticulitis is a condition affecting the large intestine or bowel. It is inflammation, occasionally infection, of diverticula, which are bulging pouches that can form in weak parts of the lining of the digestive system, most commonly in the large intestine. Diverticula are common and often harmless, normally located in the lower-left side of the colon but they can occur anywhere. Diverticulosis is simply the presence of diverticula; this doesn’t need to be treated but it can lead to diverticulitis. Diverticulitis and diverticulosis together are referred to as diverticular disease.

What causes diverticulitis?
Diverticulitis occurs when weak parts of the colon give way under pressure allowing pockets to form, protruding from the walls, called diverticula. If these diverticula tear, they become inflamed and potentially infected.
It is more likely to occur in those who do not get enough fibre in their diet. Lacking fibre in the diet can lead to constipation, increasing the pressure in the colon and increasing the risk of diverticula tearing.
It is unproven what causes diverticulitis but some studies suggest that genes may also be a factor.
What risk factors increase the likelihood of developing diverticulitis?
While the exact causes of the condition are unknown, the following factors can increase a person's likelihood of developing diverticulitis:
- Being over the age of 40
- Being overweight or obese
- Smoking
- Not getting enough exercise
- Having a diet high in fat, low in fibre
- Taking certain medications, such as NSAIDS, steroids and opioids
Men are more likely than women to develop diverticulitis.
What are the symptoms of diverticulitis?
Diverticulitis symptoms include:
- Severe, constant tummy pain, most likely to be on the left side of the abdomen.
- Feeling sick/vomiting
- Fatigue (feeling tired)
- Blood in your stool
- Constipation
- A high temperature (over 38 degrees Celsius)
- Swelling and bloating
These symptoms are common to many other gastrointestinal diseases so having one or more does not mean a person has diverticulitis.
When is medical help required?
If you experience unexplained and constant symptoms of diverticulitis, without any previous diagnosis of diverticular disease, you should contact your GP as soon as possible. If you have a previous diagnosis of diverticular disease the symptoms can be managed and treated from home. However, if you notice bleeding, or are experiencing severe pain, it is best to seek medical attention.

How is diverticulitis diagnosed?
If symptoms of diverticulitis present, it is important to visit a doctor who will take a detailed medical history, and assess symptoms, diet, bowel movements and current medication.
Additionally, a number of the following tests may be done:
- Blood tests
- Stool samples testing to check for abnormal parasites
- Digital rectal exam
- CT scans
- Barium enema which is a technique that involves inserting a liquid into the anus to highlight irregularities on X-rays
- Sigmoidoscopy, where a tube with a camera on the end that is used to give a visual inspection of the sigmoid colon and rectum
- Colonoscopy is a similar technique to the sigmoidoscopy but that offers a full examination of the colon.
- Angiography to determine where bleeding is coming from if necessary
What is the treatment for diverticulitis?
If the symptoms of diverticulitis are mild, a doctor will prescribe oral antibiotics. Additionally, resting, increasing fibre intake, and the use of over-the-counter pain medication can help to relieve the pain. If symptoms are more severe, a patient may be admitted to a hospital to have antibiotics administered through injections, and an intravenous drip to provide hydration and nourishment.
If you have already been diagnosed with diverticular disease, a high-fibre diet may help to ease any symptoms you experience with the condition. The ideal amount of fibre for an adult is 30g per day, and your doctor will discuss targets and ways to include fibre in your diet.
In more severe cases or cases of reoccurring diverticulitis that has not responded to other treatments, surgery may be considered to prevent complications from developing. Surgery normally involves removing part of the colon either through an open or minimally invasive laparoscopic procedure, and the remaining part is reattached to the rectum. In some instances, a colostomy may be required. Before any surgical procedure, the surgeon will discuss the benefits and risks with the patient.
What complications can occur as a result of diverticulitis?
Complications occur in approximately 1 in 4 cases. Common complications include:
- Abscesses, a collection of pus caused by bacterial infection in the abdomen
- Blockage or narrowing of the colon which can result in constipation and further infections
- Fistula, an abnormal tunnel-like passage way through tissue connecting the colon to a different part of the body like the skin.
- Peritonitis, a potentially life threatening condition, where puss or infection leaks from the colon into the abdominal cavity.
- Continued rectal bleeding due to blood vessel damage when diverticula burst or tear.
These complications require surgery to be treated.
How can diverticulitis be prevented?
Diverticulitis can be prevented by frequent bowel movements and an overall healthy lifestyle. Methods of achieving this are:
- Having a high fibre diet
- Exercising frequently
- Drinking plenty of water
- Avoiding or quitting smoking