Autoimmune Hepatitis – when the body attacks its liver
Autore:The human body has the potential to become confused and believe that some of our cells are not our own, and as a consequence, it begins to attack them. In the context of the liver, this is called autoimmune hepatitis. Professor Roger Williams CBE has a wealth of experience in dealing with this illness, and here he provides what you need to know about this life-threatening condition.
What is autoimmune hepatitis and what causes it?
Autoimmune hepatitis is a condition in which a patient’s immune system doesn’t recognise its own liver cells. As a result, it starts to attack them. This attack causes inflammation (hepatitis) and damage such as scarring or liver failure.
The exact cause is unclear, however autoimmune hepatitis can be associated with other autoimmune conditions such as rheumatoid arthritis , thyroiditis , Sjogren’s syndrome and ulcerative colitis .
Who is most susceptible to autoimmune hepatitis?
The textbook description of a patient with autoimmune hepatitis is a 40-50 year old woman who has become ill with jaundice.
The condition is more common in women, but it affects both sexes and a wider age group, such as children and the elderly.
What are the symptoms?
There is a spectrum of visibility when it comes to symptoms:
-
On one end of the spectrum, a patient might be entirely asymptomatic. This means that there are no visible symptoms to signify that there is an illness.
-
On the other end of the spectrum, a patient might have clear signs that they are suffering from liver problems, such as those with jaundice .
-
In the middle of the spectrum, there are symptoms that are noticeable but that don’t have a clear cause; fatigue, lethargy, some weight loss and/or potentially being abnormally underweight.
While sometimes a patient may appear entirely asymptomatic, it is well documented that at the time of diagnosis around 30% of patients have cirrhosis (a scarring of the liver tissue). This indicates that there has been a progression of serious liver damage for quite some time before the patient received a diagnosis.
Autoimmune hepatitis is often asymptomatic and not usually diagnosed until the sudden appearance of severe symptoms from end-stage liver disease, also known as chronic liver failure:
-
Ascites - a build-up of fluid in the abdomen.
-
Variceal bleed – when liver scarring or blockages disrupt regular blood flow and cause a swollen vein which then ruptures.
-
Encephalopathy – changes in the brain that occur when the liver fails to remove harmful toxins, which then reach the brain and can cause confusion, sleepiness, anxiety, fatigue and in extreme cases seizure.
How is it diagnosed?
In the majority of cases, diagnosing autoimmune hepatitis is straightforward.
Your doctor will conduct a blood test and will look for specific criteria:
-
Smooth muscle antibodies – these are produced by the body’s immune system and found in the blood. They mistakenly attack the soft muscle tissue of the liver.
-
High serum globulin levels combined with moderately raised serum bilirubin - these two compounds assist in liver function.
-
High transaminase levels – an enzyme that when high, can indicate liver damage.
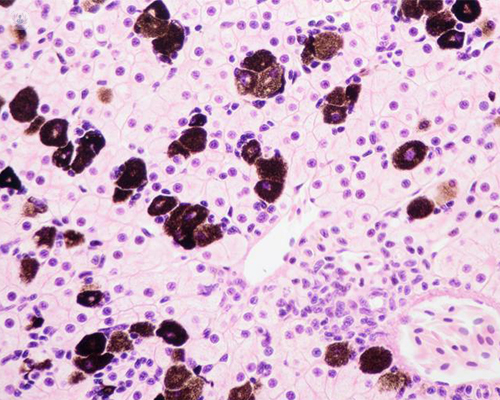
Your doctor will also conduct a liver biopsy, which is essential in establishing the diagnosis and assessing the prognosis of the patient.
How is autoimmune hepatitis treated?
When the condition is diagnosed and therefore treated in its early stages, the main method of treatment is the use of corticosteroids. These are a type of steroids with man-made hormones that are anti-inflammatory and suppress the immune system:
-
Initially, prednisolone is given at a daily dosage of 40 – 60mg and is then reduced to a lower dose of 15mg a day.
-
Budesonide has less severe side effects and is often tried long-term in patients.
-
Azathioprine is often added to treatment to reduce the chances of the steroid’s side effects, particularly osteoporosis.
In cases where patients do not respond to corticosteroids, disease-modifying drugs such as Mofetil Mycophenolate (Cellcept) are often tried along with the powerful immunosuppressant drug Tacrolimus (Prograf) - the fall back agent. Another agent Rituximab which depletes B cells in the liver has been shown to be of value recently, particularly in those with cholestasis (a decrease in bile flow) and with primary biliary cholangitis, which share similar characteristics.
When the condition is already in its later stages and showing complications of end-stage liver disease, such as the previously mentioned ascites, variceal bleeds and encephalopathy, liver transplantation can successfully restore the patient to good health.
Patients with autoimmune hepatitis need long-term expert care and one should be followed in a specialist hepatology unit.
Professor Roger Williams CBE has extensive experience in dealing with many liver conditions. If you or someone you know is concerned about their liver, pancreas, gallbladder, and/or biliary tree, don’t hesitate to book a consultation via his profile .


