Cirrhosis
Professor Kevin Peter Moore - Hepatology (liver specialist)
Created on: 11-13-2012
Updated on: 07-19-2023
Edited by: Kate Forristal
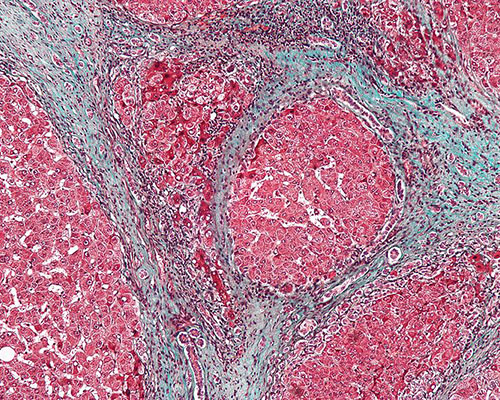
What is cirrhosis?
Cirrhosis is a disease in which the liver gradually deteriorates due to chronic injury and scarring which results from a variety of factors. The liver has the ability to repair itself, so each time the organ is injured, scar tissue is formed during the healing process. As cirrhosis progresses, more scar tissue is formed, partially blocking blood flow through the liver.
In general, liver damage caused by cirrhosis is irreparable, although early diagnosis of cirrhosis can limit or even reverse the damage.
There are different types of cirrhosis:
- Alcohol-related cirrhosis: this is caused by excessive alcohol consumption and is the most common cause of cirrhosis.
- Hepatitis-related cirrhosis: this is caused by the hepatitis virus, making the liver inflamed.
- Cryptogenic cirrhosis: it is referred to as this when the cause for the cirrhosis is unknown.
- Primary biliary cirrhosis: the immune system causes cirrhosis by mistakenly attacking healthy liver cells, which are subsequently replaced by scar tissue.
- Secondary biliary cirrhosis: causes blockage of the bile ducts.
- Sclerosing cirrhosis: the bile duct narrows, preventing the bile from flowing out.
What's the outlook for patients with cirrhosis?
Cirrhosis is an incurable disease which, if it progresses without a correct diagnosis, can lead to serious complications such as:
- Portal hypertension: high blood pressure in the veins of the liver. Blood flow is reduced, which increases the pressure in the vein that carries blood from the intestine to the liver.
- Swelling in the legs and abdomen: portal hypertension can lead to oedema and ascites, i.e. fluid formation in the legs and abdomen respectively. Both conditions may also be due to the liver's inability to generate the necessary amount of protein in the blood.
- Splenomegaly: an enlarged spleen. A decrease in the number of white blood cells and platelets in the blood may be a sign of cirrhosis.
- Bleeding: portal hypertension can cause the blood to flow into small veins, causing them to increase in size and possibly rupture, leading to severe bleeding. This bleeding is potentially fatal if the veins in the lower oesophagus (oesophageal varices) or stomach (gastric varices) rupture.

Other complications include:
- Jaundice: the skin becomes yellow due to the inability of the liver to remove bilirubin.
- Malnutrition: cirrhosis can hinder the absorption of nutrients, leading to weakness and weight loss
- Infections: cirrhosis reduces the body’s ability to fight infections.
- Hepatic encephalopathy: an accumulation of toxins in the brain, which can cause mental confusion.
- Osteoporosis: in some cases, people with cirrhosis lose bone strength and are more prone to factures
- Increased risk of liver cancer.
- Acute or chronic liver failure
What are the symptoms of cirrhosis?
One of the main problems with cirrhosis is that there are often no signs or symptoms until the disease is quite advanced and liver damage is significant. Some of the most common symptoms of this disease are:
- Tiredness
- Bleeding easily
- Itchy skin
- Jaundice
- Ascites
- Bruising easily
- Loss or lack of appetite
- Low sex drive
- Nausea
- Swelling in the legs
- Drowsiness
- Weight loss
Which specialist treats cirrhosis?
The specialists who diagnose and treat cirrhosis are hepatologists.
What are the stages of cirrhosis?
There four stages of cirrhosis. They are steatosis, scarring (or fibrosis), cirrhosis and hepatic failure.
Steatosis is characterised by:
Inflammation of the bile duct or liver - abdominal discomfort is the first symptom of inflammation. Stage I symptoms are generally curable and treatment can prevent liver disease from developing. However, symptoms like this may not manifest.
Fibrosis of the liver:
Stage II is the point where most people realise they have it. Scarring and damage from inflammation starts to obstruct the natural flow of the blood in the liver, which can cause the liver to function improperly.
Cirrhosis of the liver:
The advancement of liver disease is the cause of cirrhosis and its development. This is where scar tissue replaces the healthy liver tissue, and makes blood flow through the veins and into the liver impossible.
Hepatic failure:
This signifies the liver's function ending. In order to avoid fatalities, it requires urgent medical attention.
What is primary biliary cirrhosis?
Primary biliary cirrhosis is a type of liver disease that requires treatment, as it can get worse over time. It's caused by the immune system mistakenly attacking the bile ducts. Complications can include osteoporosis, portal hypertension, ascites, vitamin deficiencies and an increased risk of developing liver cancer.
What is NASH cirrhosis?
NASH cirrhosis is when the liver has been damaged by non-alcoholic fatty liver disease (NAFLD). NASH cirrhosis is the most severe stage of NAFLD, where inflammation leads to the liver shrinking and becoming scarred and lumpy. The damage is permanent and can lead to liver failure.
What are the skin problems related to cirrhosis?
There are various skin problems related to cirrhosis. These are:
- Jaundice, or yellowing of the skins or eyes
- Age spots
- Eczema
- Itchy skin, also know as pruritus
- Porphyria cutanea tarda (PCT) - this a skin condition that can lead to blisters, scarring and change in skin colour, alongside sun sensitivity. It's caused by a build up of proteins in the liver called porphyrins. They enter the bloodstream, and that's when problems are caused.
Can cirrhosis be prevented?
The best way to prevent cirrhosis is to take care of your liver. Therefore, you should:
- Avoid drinking excessive amounts of alcohol
- Eat a healthy, balanced diet
- Maintain a healthy weight
- Reduce your risk of getting hepatitis by having protected sex and not using illicit drugs, particularly those that are injected. There is also a vaccine now available for hepatitis B.
How is cirrhosis treated?
Treatment for cirrhosis will vary depending on the cause of the disease and whether other complications are present. The aim of treatment is to slow the progression of scar tissue in the liver. In the event of complications, hospitalisation may be necessary.

The main treatments for cirrhosis are:
- Eating a nutritious diet.
- Avoiding alcohol and other substances that can affect liver function.
- Diuretics are recommended for oedema and ascites.
- Beta-blockers that lower blood pressure may be prescribed for portal hypertension.
- Hepatic encephalopathy is treated by cleansing the intestine with lactulose.
- People with cirrhosis and hepato-renal insufficiency should have haemodialysis.
- Liver transplant. In advanced cases of cirrhosis where the liver stops working, liver transplantation may be the only option. With transplantation, the diseased liver is replaced with a healthy liver from a deceased donor, or with part of the liver of a living donor.