Subdural haematoma
Professor Andrew McEvoy - Neurosurgery
Created on: 11-13-2012
Updated on: 04-19-2023
Edited by: Jay Staniland
What is a subdural haematoma?
A subdural haematoma is an accumulation of blood in the skull or within the brain tissue that is caused by a blood vessel rupture in the brain. This can come on suddenly or develop over time. It’s often caused by trauma to the head from a fall or severe blow such as from a car accident.
A subdural haematoma can be fatal and requires immediate treatment to remove blood that has collected in the brain tissue or under the skull, as it puts pressure on the brain.
Prognosis of subdural haematoma
There are some head injuries that can be minor, such as a concussion, in which the patient may lose consciousness for a short period. However, a subdural haematoma can cause death, since the blood from the injury collects within the skull and can put pressure on the brain.
Symptoms of subdural haematoma
The signs and symptoms of a subdural haematoma can show immediately after the trauma or take some time to appear. When the visible signs are delayed, it can take days, or even weeks to show - this period is called a lucid interval - although with time the brain pressure will increase and the symptoms will appear eventually.
Some of the most common symptoms of a subdural haematoma are the following:
- headache which gradually increases in intensity
- vomiting
- drowsiness
- progressive loss of consciousness
- dizziness
- confusion
- slurred speech
- unequal pupil size
As more blood flows to the brain, or the space between the skull and the brain, other symptoms such as seizures, lethargy or unconsciousness may appear.
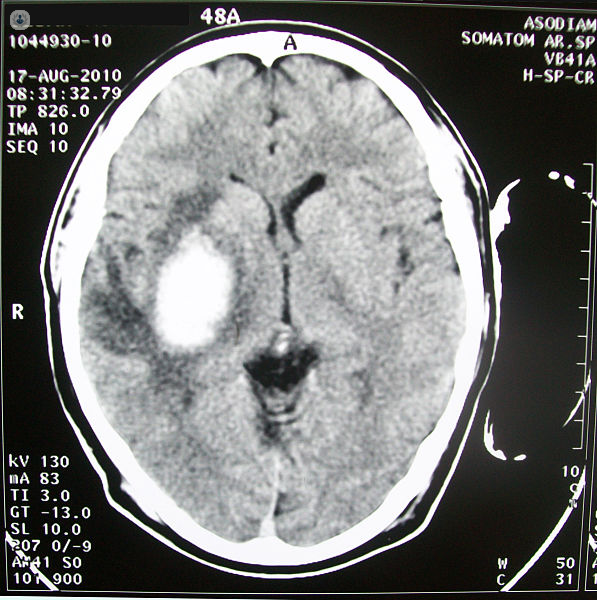
Diagnosis of subdural haematoma
The diagnosis of a subdural haematoma can be complicated, since the patient may appear to be fine, despite having a head injury.
However, losing consciousness after suffering trauma is linked to a haematoma, unless the evidence indicates otherwise.
Diagnostic image tests are the best way to check the position and size of the haematoma. These include:
Causes of subdural haematoma
The causes of subdural haematoma are very clear; a head injury is the frequent cause of intracranial bleeding, usually occurring due to an accident or fall.
There are three types of subdural haematomas: acute, sub-acute and chronic.
- Acute – this is the most dangerous and is caused by a serious head injury. The signs usually appear immediately.
- Sub-acute - symptoms can take days or weeks to manifest after your injury
- Chronic – this is usually the result of less severe head injuries. It can cause slow bleeding and the symptoms are usually delayed up to months. It can be caused by a small bump to the head, such as from getting in and out of the car. You may even recall the injury.
The risk of suffering a subdural haematoma increases with age. People who take aspirin or other forms of blood-thinning medication, or consumers of excess alcoholic beverages are at greater risk of developing this.
All three types require immediate medical attention so to prevent brain damage and/or death.
Prevention of subdural haematoma
There is no way to prevent the occurrence of an subdural haematoma if it is caused by an accident. However, you can try to minimise or avoid head injuries using the following precautions:
- Wear a helmet when playing contact sports, cycling, motorcycling, skiing, skating, snowboarding or doing any activity that could result in a head injury.
- Always wear a seat belt when you are in a motor vehicle.
- Protect young children by using a properly fitted car seat, adding padding to table corners, block stairways, and prevent children from climbing onto high or unstable objects.
Treatment for subdural haematoma
Subdural haematomas usually need to be treated with surgery to drain the haematoma as soon as possible. If the haematoma is small and shows no symptoms, then it isn't necessary to remove it. However, signs and symptoms can appear days or weeks later, so the patient should be under observation to control any neurological changes.
If the patient takes any blood-thinning medications, treatment may be necessary to reverse the effects of the medication and reduce the risk of bleeding.
