Duodenal switch procedure – switching things up in weight loss surgery
Escrito por:The traditional biliopancreatic diversion with duodenal switch (BPD/DS) procedure restricts the amount of food you can eat, and also reduces the amount of nutrients your body can absorb. However, whilst it is effective in enabling patients to lose weight, there are concerns regarding vitamin and protein malnutrition due to the amount of small intestine removed. Mr Kesava Reddy Mannur, a top surgeon, explains what the newer, modified version of BPD/DS surgery involves (the DS/SADI procedure).

What is the duodenal switch procedure? What does it treat?
The modified BPD/DS procedure also combines restrictive and malabsorptive elements to achieve and maintain the best-reported long-term percentage of excess weight loss among modern weight-loss surgery procedures. This is performed laparoscopically, giving all the benefits of laparoscopic surgery. It is performed in two major steps:
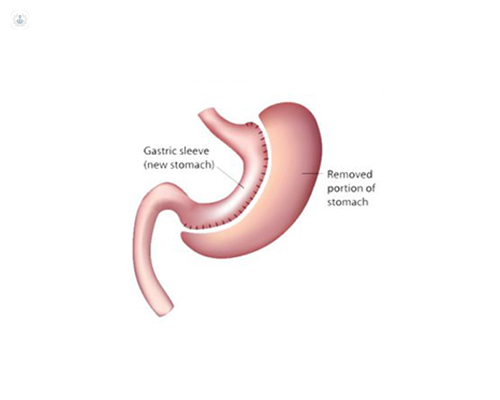
- The Restrictive Component (sleeve gastrectomy)
This stage of the operation involves removing three-quarters of the stomach, leaving the stomach in the form of a narrow tube. Also remaining is the pyloric valve (this releases food into the small intestine) and a section of small intestine that connects to the stomach (i.e. the duodenum).
- The Malabsorptive Component (distal bypass) – Actual DS/ SADI
It is like doing gastric bypass but at the duodenum level instead of the stomach. The small bowel is divided near its middle (about 250 to 300 centimetres from the ileo-caecal valve) and the distal divided small bowel (alimentary limb) is joined to the proximal divided duodenum (just beyond the pylorus, stomach outlet). In SADI, we leave there without any further joining as follows in DS.
The proximal part of the divided small bowel (biliary limb) is joined to the distal bowel about 100 centimetres from the ileo-caecal valve (junction of the small and large bowel). Thus, the malabsorptive component of the DS procedure rearranges the small intestine to separate the flow of food from the flow of bile and pancreatic juices for a long distance. This inhibits the absorption of calories and some nutrients. Further down the digestive tract, these divided intestinal paths are rejoined; food and digestive juices begin to mix, and limited fat absorption occurs in the common tract as the food continues on its path towards the large intestine.
Sugars, protein and nutrients are absorbed to a limited degree in the food tract. Fat absorption occurs only in the common tract. Therefore, the shorter the common tract, the less fat absorption can occur.
Advantages of the DS/SADI approach:
The DS/SADI procedure keeps the pyloric valve intact. This eliminates the possibility of dumping syndrome, marginal ulcers, stomal strictures and blockages, all of which can occur after other gastric bypass procedures. The preservation of the pylorus means the food is allowed in very small quantities into the small bowel from the stomach, in a softer consistency. As a result, the DS procedure enables more normal absorption of many nutrients, including protein, calcium, iron and vitamin B12 than is seen after gastric bypass procedures. The stomach will eventually (after 12 to 18 months or so) expand to hold a small- to near-normal-sized meal, with weight loss being maintained by the malabsorption component of the procedure. It hardly has any hypoglycaemia, unlike the gastric bypass; insulin level increase is minimal with DS, whereas it is enormously raised in gastric bypass.
How long does duodenal switch surgery take?
It takes about 1.5 hours to do the DS component and one hour to do the SADI component (if the sleeve gastrectomy was done before). If they are done together with sleeve gastrectomy, then it will take about two hours to do DS and 1.5 hours to do SADI-S.
Are there any side-effects or complications related to the duodenal switch procedure?
Following DS/SADI-S, possible complications are:
- Leaks from anastomosis: these are rare because of the way it is done. If this happens, one feels severe pain in the abdomen and doesn’t move for fear of pain the next day. Diagnostic laparoscopy has to be done urgently and the leak must be repaired.
- Bleeding is extremely rare; most of the time one requires a blood transfusion if bleeding does occur.
- Chest complications, such as pneumonia can occur as after any surgery; this is prevented by deep breathing exercises, coughing, and early mobilisation.
- Deep vein thrombosis (DVT) - clots in the legs or pulmonary embolism can happen; these are prevented by early mobilisation, leg compressions, and blood thinners.
- Late complications of an internal hernia are rare; one would complain of recurrent, colicky abdominal pain. Diagnostic laparoscopy has to be performed urgently and any internal hernia has to be repaired.
- In general, a shorter common tract means that patients might experience more of the side-effects that can affect all distal bypass patients (e.g. smelly gas, diarrhoea, vitamin, iron and calcium deficiencies, protein malnutrition). Patients have to understand the operation well to adjust their lifestyle, with special attention to their diet to avoid this.
What special measures are taken during recovery from duodenal switch surgery?
Most patients stay in hospital for one day if DS/SADI is done alone without sleeve gastrectomy and two days if sleeve gastrectomy is combined with DS/SADI. If DS/SADI is done alone, you will need to be on a liquid diet for one week and then on a soft food diet during the second week. After this, a solid diet can be resumed. If DS/SADI-S is done along with sleeve gastrectomy, then one has to follow the guidelines of sleeve gastrectomy – a fluid diet for 4 to 6 weeks, followed by a soft diet and then a solid diet. If nutritional deficiencies are a problem, the digestive and absorptive area has to be increased by lengthening the common channel where digestion happens.
They have to reduce fat intake to prevent diarrhoea and foul smelling gas. One has to take more protein intake (90 to 120 grams instead of usual 60 gram). You will also have to have vitamin and mineral supplements, as well as taking up exercise to prevent loss of muscle mass and bone density.
If you would like to schedule a consultation with Mr Mannur, you can go to his Top Doctors profile and request a visit.


