Whiplash injuries: managing neck pain
Written by:Whiplash is a neck injury caused by sudden movement of the head. It can often happen after a slip, fall or car accidents.
Dr Shankar Ramaswamy, a leading consultant in anaesthesia, pain management and neuromodulation (who is based in London and Kent) recently spoke with us to give advice on how to manage neck pain from whiplash.
What is whiplash injury?
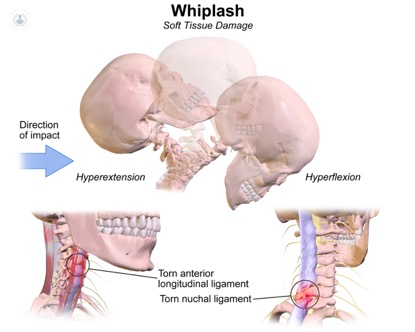
Whiplash is a neck injury caused by a sudden movement of the head. It typically occurs following a sudden or excessive movement resulting in hyperextension, hyperflexion, or rotation of the neck. It causes neck pain and other associated symptoms. Whiplash injury can occur following a road traffic accident or may also be caused by sports injuries, falls or assaults.
Whiplash-associated disorders (WAD) is defined by the Quebec task force as: ‘Whiplash is an acceleration-deceleration mechanism of energy transfer to the neck.
Incidence of WAD?
Incidence of WAD is about nine per 1000 people in the UK. Over 90% of WAD usually occurs at low speeds of < 14 mph due to rear-end, low-impact collisions.
Studies suggest that in over 60% cases, the source of the pain in WAD is the zygapophysial (facet) joints (especially C2/3 and C5/6 levels), rather than the muscles.
Types of injury resulting in WAD?
Whiplash can occur due to two types of injuries:
A slow-moving or a stationary vehicle stuck from behind: This results in hyperextension injury to the driver and the passengers in the vehicle. As a consequence, the body is thrown forward while the head lags behind. This results in the hyperextension of the neck. After the head and neck reaches maximum extension, the neck will then snaps into flexion.
Deceleration injury when the fast-moving vehicle suddenly halts: This will throw the head forwards and flexes the cervical spine. Hyperextension can occur in the subsequent recoil.
What are the grades and symptoms of whiplash?
Whiplash-associated disorders (WAD) can be classified by the severity of signs and symptoms:
Grade 0:
No complaints of neck pain or stiffness, asymptomatic, absent physical signs.
No investigations or treatment required.
Grade 1:
Neck complaints: pain, stiffness, or tenderness of the neck. No physical signs.
No investigation required and best managed with simple pain killers such as paracetamol/ NSAIDs.
Grade 2:
There is a combination of neck complaints and musculoskeletal signs. Patient reports neck pain, stiffness.
On examination, there is tenderness of the neck. Musculoskeletal signs include decreased range of movement and point tenderness of the neck.
A plain X-ray of the cervical spine is not routinely indicated unless suspected bony injury, impaired consciousness leading to masked pain sensation, high speed/impact collision.
Grade 3:
There is a combination of neck complaints and neurological signs.
Patient reports neck pain, stiffness, or tenderness of the neck. Neurological examination shows sensory deficits, motor weakness, and/or decreased or absent deep tendon reflexes.
Specialist imaging is often indicated and the patient may need stronger analgesics.
Grade 4:
Neck complaints and fracture/dislocation:
Patient reports neck pain, stiffness, or tenderness of the neck along with dislocation or fracture with or without spinal cord injury.
How is it diagnosed?
History: of trauma/ injury due to excessive neck flexion, extension or rotation. Typically reports headache, neck pain, referred pain to shoulder or arms.
Examining: evidence of muscular spasm, restricted range of movements in the neck, tenderness points, and neurological problems in the upper or lower limbs including weakness, numbness, sensory changes.
Red flags: rule out features suggestive of a serious spinal or other abnormality, including compression of the spinal cord (myelopathy), cancer, severe trauma or skeletal injury, and vascular insufficiency.
Investigation: Important to avoid unnecessary/ over investigation as the vast majority don’t need any imaging. The commonest associated finding is pre-existing degenerative cervical spine disease (especially spondylosis at the C5/6 level). Common radiology imaging includes cervical X-ray, CT scan, MRI, CT myelogram.
MRI is indicated if there are neurological signs or if other assessments show ligamentous and disc injury.
How long can the pain from whiplash last?
Outcome of WAD
Typically, whiplash is a self-remitting condition which gradually gets better in about 2 to 3 months. But up to 40% of patients with WAD suffer from symptoms beyond three months (chronic whiplash) and could remain so even up to 2 years. Up to 2–4.5% of patients are left permanently disabled.
Factors influencing outcomes:
- Severity of injury
- Yellow flags: To identify other conditions that could affect the outcome such as anxiety, depression, OCD, somatisation.
- Ongoing litigation seeking compensation can also have an impact on the outcome.
What treatment is available to manage the pain caused by whiplash?
In the absence of severe injury (Grade 0-2 and mildly symptomatic grade 3): Reassurance, encouragement for early mobilisation, physiotherapy with isometric exercises are essential to have good long-term outcomes.
Bed rest and immobilisation of the neck with a soft collar should be avoided.
Patients with severe injury may need intravenous steroids in the acute stage (in the first few hours).
Multimodal pain management strategies including pharmacotherapy, physical therapy and psychological therapies, patient education and self-management strategies should be considered.
A chronic whiplash injury may need specific interventions such as cervical medial branch block, cervical medial branch radiofrequency neurotomy/ denervation. Other interventions such as Trigger point injection, botulinum toxin injections have been used, but the evidence supporting such treatment is limited. If there are features of nerve type pain, antineuropathic agents as per NICE guidelines NG59 should be considered.
Patients with more severe injury with neurological deficit may need surgical treatment.
Are some treatments more effective than others?
Reassurance, encouragement for early mobilisation and physiotherapy should be strongly advocated over bed rest, immobilisation of the neck with a soft collar even if it is painful.
For more information about pain management, you may like to book an appointment or e-Consultation with a leading pain management specialist such as Dr Shankar Ramaswamy.


