An expert explains the treatment of retinal vein occlusion
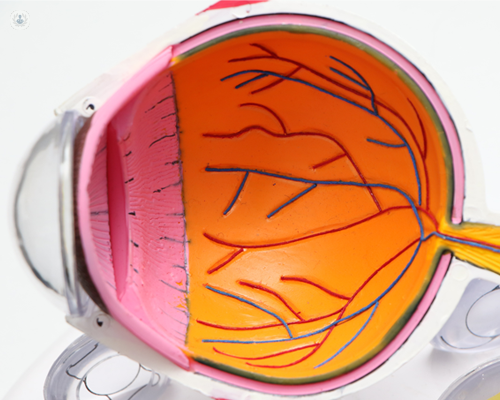
Written by:The retina is a thin layer of tissue at the very back of the eye, made up of different types of cells which allow us to see. It is responsible for interpreting light which is transmitted to the brain to form an image. If a blockage occurs in a vein of the retina, it can lead to a deterioration of one’s vision. Highly-esteemed, London-based consultant ophthalmologist Mrs Samantha Mann, who specialises in the treatment of conditions affecting the retina, shares her expertise on retinal vein occlusion.
What is retinal vein occlusion? Is it serious?
A vein occlusion is when there is a blockage of one of the veins at the back of the eye on the retina. The retina is the very thin film on the inner surface of the back of the eye that allows us to see. This blockage can occur in one of the branches of the main veins, called a branch retinal vein occlusion (BRVO), which can cause loss of vision in either the top or bottom part of your sight. The blockage can also occur in the main central vein, which is called a central retinal vein occlusion (CRVO) which tends to be more serious resulting in loss of vision in the central area. Although both of these conditions can result in reduced vision, the majority of these can be treated if diagnosed early, although treatment is often for a prolonged period of time.
What is the most common cause of retinal vein occlusion?
The blockage in the vein is often due to a blood clot that obstructs the blood flow in the vein. The most common conditions that are associated with venous occlusions are:
- high blood pressure
- high cholesterol
- glaucoma- high pressure in the eye
- diabetes
- smoking
- certain rare blood disorders
Can you go blind from retinal vein occlusion?
It is rare to totally lose your vision from vein occlusions but swelling often occurs from damaged blood vessels at the central part of the retina, causing blurring of central vision. This swelling can be treated with anti-vascular endothelial growth factor (anti-VEGF) or steroid medications. If. If the blood supply is very damaged at the back of the eye following a vein occlusion, it is possible for the vision to be reduced permanently. This is due to abnormal blood vessels growing towards the front of the eye, blocking drainage of fluid from the eye, and causing a rise in pressure. If this occurs, laser treatment may be required to reduce the growth of the blood vessels.
Can retinal vein occlusion go away on its own?
Some forms of branch retinal vein occlusion, if mild, can get better on their own over a few months, as the eye recovers. Most vein occlusions, particularly central retinal vein occlusions, require some treatment to be given, at least for a few months.
Is there any cure for retinal vein occlusion?
Unfortunately, there is no way to unblock the venous occlusion, but the swelling of the retina and any growth of abnormal blood vessels can be treated to improve and stabilise the vision over the long term.
What is the best treatment for retinal vein occlusion?
The best treatment for venous occlusion depends on the extent of the occlusion and whether the damaged vessels have resulted in swelling of the central part of the retina. Anti-VEGF injection treatment or steroid injection treatment into the eye have been shown to be effective at reducing the leakage at the back of the eye and improving vision. These injections, however, have to be repeated regularly as the effect of the drug wears off usually after four-to-eight weeks. These injections can safely and quickly be given into the eye as an outpatient without too much discomfort.
If abnormal blood vessels grow towards the front of the eye (which usually occurs more frequently in CRVO), laser treatment may need to be applied to the retina. Again, this can be carried out easily as an outpatient. Although the laser treatment does not improve the vision, it can help to stabilise it.
Retinal vein occlusion can cause serious damage to your vision if it is left untreated. If you are experiencing any of the symptoms mentioned above and would like to book a consultation with leading London-based consultant ophthalmologist Mrs Samantha Mann, you can do so by visiting her Top Doctors profile today.


