An expert's guide to pH testing
Written by:If you’re experiencing chronic heartburn symptoms or pain in your chest that can’t be explained by heart or lung problems, you could be eligible for pH testing. It’s a procedure that assists in the diagnosis of gastro-oesophagal reflux disease.
Here to provide a detailed guide to this test is highly-regarded consultant physician and gastroenterologist Mr Owen Woghiren.
What is pH testing?
So, pH testing is a method by which we measure the amount of acid which is produced in the upper digestive tract in the stomach. Acid is produced in the stomach by the cells, which are specialised cells, so these cells can sometimes produce too much acid and that can cause symptoms. So when doctors send you for pH testing, they're trying to determine how much acid that is actually produced in your stomach, and whether that's actually causing, or a cause of, your symptoms.
What can it help to diagnose or point to?
So, when we want to measure the acid production in your digestive system, it usually means that you're having some symptoms which are thought to be due to acid production. So, symptoms such as:
- Heartburn;
- Or just general digestive symptoms, with a lot of pain in the epigastric area, which is just beneath the breast bone.
We also measure the acid production in cases where somebody has chest pain which isn't thought to be coming from the heart or lungs. That's a syndrome or condition called atypical chest pain. So, atypical chest pain means that your chest pain isn't coming from the usual areas of your anatomy like your chest, or your heart, and it's thought that it might be coming from maybe your muscular skeletal system, or even your oesophagus or your food pipe, your digestive tract. And this can be caused by excessive acid production. So, we use it to investigate people who have heartburn which isn't responding to conventional treatment or people who have chest pain which we feel might be coming from the digestive tract.
Heartburn is a sensation that you get behind your breastbone and your chest. Atypical chest pain is a vague pain of unknown cause. Sometimes, when somebody presents with chest pain that you don't know, with the investigations of the heart and the lungs, and you can't find a cause for it, then you might consider that it could be coming from the food pipe. So, that's why it's called atypical chest pain.
How is pH testing carried out?
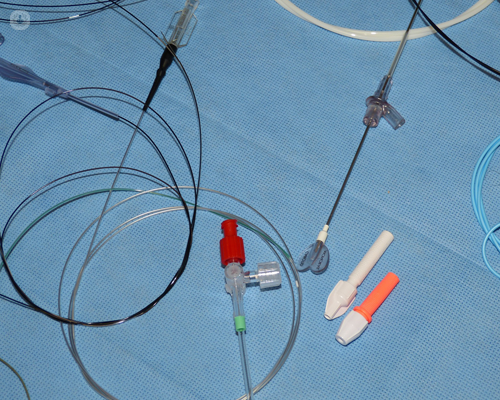
In order to measure the acid that we produce in the stomach, we have to pass what we call a pH catheter, which is a very thin tube through the nose, down into the mouth and the food pipe. And when you do that, you basically place the tube just above where the food pipe stops and the stomach begins. The whole idea is to measure to see whether any acid is being produced in the stomach and coming back into the food pipe. At the bottom of the food pipe, you shouldn't expect to see any acid there. So, if you detect that there's acid in that area, then it can help you determine that the symptoms are coming from acid which is coming back up from the stomach; what we call reflux.
Now, you are supposed to have acid in your stomach so we don't necessarily measure the acid in your stomach. What we actually do with pH testing is measure whether there's any acid production or any acid present in the lower food pipe above the stomach. So that's what we mean by pH testing. We also use it to measure the pressure around there because you have a sphincter there and if the sphincter is a bit lax, and is allowing acid to come up from the stomach, you might produce the same symptoms.
When you're measuring the acid, you correlate the symptoms which the person is experiencing with the acid production at the time. So, you produce a graph which tells you: 'Yes, this is how much acid which was produced at a certain time.' And you try and correlate that with the symptoms, which the person having the test would show. So, if a patient is having a test done, it's usually done over a 24-hour period.
In this period when the patient has the tube down their nose, into the food pipe, if they have any symptoms, I will press a button which records the acid production in that area at that time. So that's why it's done over 24 hours. We can help determine whether the acid production or the acid in that area is of a significant level to produce your symptoms, and whether it actually correlates with your symptoms. Some people do have acid coming back into the food pipe but it doesn't correlate with their symptoms and that makes us think of other reasons why they might be having chest pain or heartburn.
When will my doctor refer me for a pH test?
Like I mentioned earlier, when we're not quite sure what the cause of your symptoms are, we will consider this pH testing. Normally when somebody has heartburn, we'll perform a gastroscopy, which is a test where we look into the food pipe and into the stomach to see if there's any cause for your symptoms like a hiatus hernia or even oesophagitis, which means inflammation of the lower food pipe caused by acid. So, if you've had a gastroscopy or even a barium swallow, which is a similar test which measures to see if there's any reflux, and we don't find any significant findings such as a hiatus hernia or ulcers, or anything that can attributed to these symptoms, then we'll consider pH testing.
We'll also consider pH testing when you have your chest pain which cannot be explained by other pathologies or problems. It helps us work out whether your symptoms of heartburn or chest pain are caused by the presence of acid in the lower food pipe.
What can ‘abnormal’ results point to?
An abnormal result is when you have excessive production or presence of excessive amounts of acid in the lower food pipe. That would suggest you have a condition called pathological reflux. This means that reflux can be physiological, that means we always have a little bit of reflux from time to time.
If you're having excessive reflux and it's causing symptoms, and your DeMeester score which is a way we measure the acid, or above a certain level, it would suggest the amount of acid which is refluxing from your stomach to your lower oesophagus is what we call a pathological level. That's a level that causes symptoms and a level that can also cause damage. With the pH testing, we sometimes do pressure testing in conjunction with that, and we look for the presence of a hiatus hernia.
If you were to come to me with a positive test, i.e., that your test shows that you have pathological, or excessive, reflux at the bottom of your food pipe, and you have a hiatus hernia, then we can consider you for further treatment. So, you might be considered for anti-reflux surgery and that type of treatment.
Sometimes we may put you on protein pump inhibitors to reduce the amount of acid production in the stomach. If that doesn't help, then we now start considering you for surgery. Normally, before we think of performing a surgical procedure on patients, we'd start with the anti-reflux measures such as:
- Your change in diet;
- Your lifestyle;
- Stopping smoking and;
- Alcohol consumption.
If you’re concerned about your stomach acid levels or other gastroenterology-related issues, arrange an appointment with Mr Woghiren via his Top Doctor’s profile.


