Ptosis: A droopy upper eyelid in children and adults
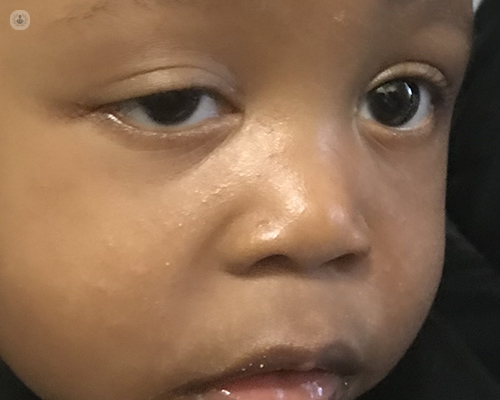
Written by:Ptosis, which refers to the drooping of an upper eyelid over the eye, is an ophthalmic condition that can be congenital or acquired in nature, and that can lead to loss of vision.
Here, Mr Danny Morrison, highly esteemed consultant ophthalmic surgeon, provides an expert insight into ptosis in children and adults, explaining causes, symptoms, treatment and more.
What is ptosis, and at what age does it typically occur?
Ptosis is a droopy upper eyelid. Ptosis that occurs in children and adults is very different, because of the different causes that lead to the onset of ptosis. Treatment also differs slightly.
Children with ptosis are usually born with it, although they can acquire it an any stage during childhood. A congenital ptosis (which is a droppy eyelid since birth) is due to a localised defect or abnormality in the muscle that raises the eyelid. This happens when the muscle (called the levator muscle) has failed to develop properly and thus, is weak. As a result, not only is the muscle not able to lift the eyelid, but problems can also occur because of poor eyelid closure.
Ptosis can affect one or both eyelids, and it is not usually symmetrical.
In most cases of paediatric ptosis, no extensive tests or investigations are required. An examination by a paediatric ophthalmologist is essential, to detect rare causes that might be trauma-related, or that may have an associated syndrome or genetic abnormality. Examples would be Horner's syndrome (a third nerve palsy) and Marcus Gunn 'jaw winking' syndrome.
Adult ptosis, on the other hand, is more typically acquired, with the commonest cause being the stretching or weakness of the levator muscle that lifts the eyelid. Like with paediatric ptosis, the causes of adult ptosis (such as, myasthenia gravis) are rare. These causes can usually be identified in clinic with an examination or occasionally with a simple blood test.
In children, ptosis is important to treat because of its impact on vision and visual development. The droopy eyelid, if it partially or completely covers the pupil, can cause permanent loss of visual acuity (clarity of vision) on the affected side.
Adult ptosis, as well as decreasing vision and disrupting the ability to see properly, can cause discomfort due to the fatigue and the extra effort used by the eyebrow or forehead muscle trying to raise the eyelid.
There is - in all forms of ptosis - the added effect where the affected individual will look sleepy or tired.
What are the main associated risk factors?
In children, there are a few common associations and risk factors. Genetic syndromes, such as Horner's syndrome or Kearns-Sayre syndrome (a generalised muscle weakness), are very rare.
In adults, one risk factor for ptosis is long-term contact lens wear, due to the upper eyelid muscle being gradually stretched and weakened over the many years of inserting and removing contact lenses.

When would ptosis be treated as a medical emergency?
Only very rarely is ptosis a medical emergency.
A droopy eyelid of sudden onset in conjunction with a persistent headache and squint (strabismus), however, can be a sign of a third cranial nerve palsy. This is immediately recognisable to an ophthalmologist and in such (very infrequent) cases, an urgent head scan is usually required.
In adults and children, recognising myasthenia gravis or Kearns-Sayre syndrome is a relative emergency, since in the case of myasthenia gravis, systemic medication treats not only ptosis, but also the general condition.
Might ptosis be a sign of a more serious underlying condition?
Only rarely is ptosis a sign of a more serious underlying condition; the majority of cases of paediatric or adult ptosis do not indicate a serious underlying condition.
However, children and adults with a new ptosis should always see an ophthalmologist.
What might be likely to happen if ptosis is left untreated?
In children, untreated ptosis can lead to the permanent loss of vision by occlusion amblyopia, known as a 'lazy eye’. In adults, untreated ptosis can cause temporary loss of vision (by obscuring the visual axis), headaches, brow-ache, and neck discomfort (from altering the head’s position to compensate).
The treatment for ptosis in adults and children is surgical. Different techniques are used, but most involve tightening or strengthening the levator muscle, or assisting the levator muscle with a 'sling' of artificial material from eyebrow to tarsal plate, such as a nylon, silicone band or thread (suture). In some instances, the sling to elevate the eyelid from the brow is created by using a graft of fascia (this is tendon-like tissue) taken from the affected individual's own leg, or from the muscle of the forehead.
Paediatric surgery is always performed under a general anaesthetic and it is usually a day-case procedure. An eye patch might be needed to be worn (over the unaffected eye for a few hours a day) for several months, before or after surgery, to strengthen the vision in the eye with ptosis.
With adult ptosis, most repairs are performed with a local anaesthetic that is injected into the eyelid. The levator muscle is then tightened and the operation is carried out as a day-case hospital procedure.
Don’t hesitate to visit Mr Morrison’s Top Doctors profile today to receive the utmost expert ophthalmic care for your, or your child’s, ptosis.


