What is Mirena coil?
Written by:What is Mirena coil?
Mirena is an intrauterine coil which releases special type of hormone called progestogen. It helps to reduce the amount of menstrual blood loss and helps with contraception.
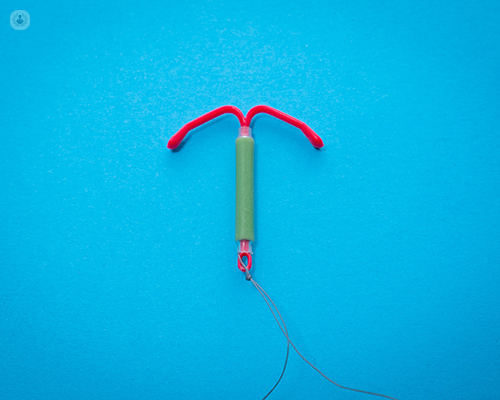
What does Mirena coil look like?
Mirena coil has a T shape structure and is quite small. It is a little smaller than size of the cavity of the uterus. It is attached to two threads which come through the cervix into the top part of the vagina.
When it is a time to remove the coil, doctors will pull the threads and the coil will come out easily.
What does it do?
Mirena has two main functions; to control heavy menstrual loss and for use as contraception.
What are the benefits of Mirena coil?
Mirena coil is used for control of heavy menstrual loss. It has significantly reduced the number of hysterectomy procedures that used to be carried out before the discovery of Mirena.
Previously, there were no other options to control heavy menstrual loss. Other surgical procedures such as hysterectomy or endometrial ablation are more invasive than Mirena coil therefore, for the majority of patients (85% or more) the coil is enough to control heavy menstrual bleeding.
It is also a contraceptive so for people who are not planning to conceive it is usually the most recommended first choice of management.
When is the best time for insertion of Mirena coil?
Mirena can be inserted at any time, but it is a little easier to insert it shortly after the end of menstrual period.
During the procedure, what does the doctor say to the patient? How can they prepare for Mirena coil?
The doctor will tell the patient to expect to have some period like discomfort during the insertion.
They recommend having something for a pain relief such as paracetamol or ibuprofen about an hour before the insertion.
What aftercare advice is there?
Immediately after the insertion there might be some mild bleeding, and period like pain therefore taking some paracetamol after insertion will be useful.
Gentle vaginal examination is recommended 6 weeks after insertion to confirm appropriate position of the coil.


