Human papillomavirus (HPV)
Mr Rahul Nath - Obstetrics & gynaecology
Created on: 11-13-2012
Updated on: 11-09-2023
Edited by: Carlota Pano
What is the human papillomavirus (HPV)?
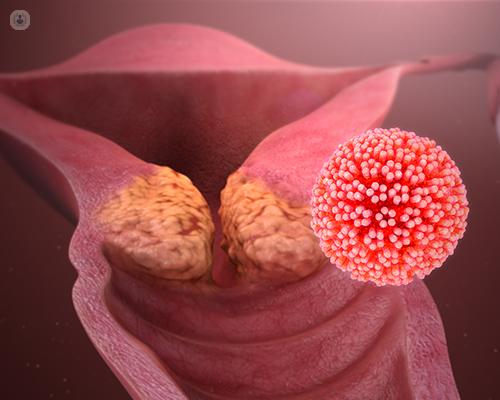
Human papillomavirus (HPV) is the term for a common group of viruses that can infect the skin and mucous membranes. There are more than 100 different types, most of them harmless, but some types are associated with an increased risk of cancer or cervical dysplasia (abnormal changes in the cells of the surface of the cervix). These are acquired through sexual contact with an infected partner and can be low or high-risk.
Low-risk strains can cause genital warts. Conversely, high-risk strains can cause cancer of the cervix, vulva, vagina and anus in women; and cancer of the penis and anus in men. High risk strains can also cause cancer at the back of the throat, called oropharyngeal cancer. Genital warts and cancer can develop months and years after getting infected with HPV.
What are the symptoms of HPV?
In many cases, HPV infections produce little to no symptoms and the infection will go away without treatment. However, whilst that person may not experience symptoms of HPV, they are still carriers of the virus and can transmit it to any sexual partners they have. HPV infections can produce genital warts or warts in the throat. High-risk strains of the virus can also cause cell abnormalities in the cervix, which can develop into cervical cancer if untreated.
Unfortunately, symptoms of cervical cancer do not usually become apparent until the cancer is in its later stages and you can have HPV for years without it causing symptoms of health issues. This is why regular cervical screening is so important for women after the age of 20-25.
What causes human papillomavirus infections?
HPV is very common and 50 per cent of people who are sexually active will contract it at some point in their lifetime.
There are several factors that increase your risk of suffering from human papillomavirus infections. Most people who become infected with the virus will do so from direct sexual contact, including oral sex. The risk is increased if you are not practising safe sex (i.e. using a condom), because HPV is transmitted by skin-to-skin contact. Another risk factor is having a depressed immune system and damaged skin areas, as open wounds are more likely to develop warts.
Can HPV infections be prevented?
It is possible to get vaccinated against the human papillomavirus to reduce your risk of being infected by the high-risk strains. This vaccine is offered to girls in school from the age of 12 and is highly recommended. Using condoms is also advised to reduce your exposure and risk of contracting HPV during sex. To prevent HPV infections from developing into cervical cancer, women should also have frequent cervical screening once they become sexually active.
What is the treatment for an HPV infection?
There is no cure for the human papillomavirus, but 80 per cent of infections will go away on their own within two years without problems. Infections that last longer are those that may lead to cancer.
Surgery can also be used to treat cervical abnormalities that result from HPV:
- Large loop excision of the transformation zone, in which abnormal cells are removed using a heated and thin wire loop.
- Cone biopsy, where a piece of tissue containing abnormal cells is cut out.
- Laser treatment that pinpoints and destroys abnormal cells.
- Cold coagulations, where a heat source burns away normal cells.
Genital warts that result from HPV may be treated with topical creams or liquids, surgery or cryotherapy.
There are many types of HPV, so there is a high risk of contracting the HPV infection again.
How is HPV diagnosed?
There's no blood test that can diagnose HPV. Rather, it is detected during cervical cancer screening, when a small sample of cells are taken from the cervix and tested for HPV.
Anal screening may be offered to men who have a higher risk of developing anal cancer, such as men with same sex partners.
HPV genital warts vs Herpes
Genital warts are, usually painless, mucous membrane growths that appear in the vagina, vulva, cervix, penis, scrotum and anus, caused by low-risk strains of HPV. This is a different type of HPV to the one that causes cervical cancer, so having genital warts won't put you at a higher risk of developing cancer. However, if warts are left untreated, they can persist and grow in size and in number.
Herpes sores, on the other hand, appear as blisters or open wounds that are accompanied by a burning sensation. Unlike genital warts, herpes is caused by a herpes simplex virus (HSV) infection.
What happens if both my partner and I have HPV?
It's still unclear how HPV works between sex partners, but current research suggests that one in four couples share the same strain or strains of HPV, even if both partners don't show symptoms. The same virus is unlikely to be passed back and forth between partners.
HPV in pregnancy
If you're pregnant and have HPV, you may be at an increased risk of developing bleeding genital warts or abnormal cervical changes. If you have HPV and genital warts, you may pass the infection on to your baby. In rare occasions, HPV may cause growths to develop in your baby's larynx.
If genital warts block your birth canal, you will need to have a C-section.
You must speak to your doctor or gynaecologist if you're pregnant and have genital warts, as some treatment methods for warts aren't suitable during pregnancy.















