Jaundice
Dr Matthew Foxton - Hepatology (liver specialist)
Created on: 11-13-2012
Updated on: 03-31-2023
Edited by: Sophie Kennedy
What is jaundice?
Jaundice, also known as icterus, is a disorder that causes the skin and white parts of the eyes to turn a yellowish colour. It is not a disease in itself, but rather a symptom of something happening. Jaundice occurs when there is an excess of bilirubin, a yellow compound which is formed by red blood cells breaking down in the body.

What are the symptoms?
The main symptom of jaundice is yellow discolouration of the skin and mucous membranes. In some cases, other symptoms such as coluria (very dark urine) and acolia (very light stools due to the absence of pigments derived from bilirubin) may occur.
Further symptoms of jaundice include:
- Fever
- Chills
- Abdominal pain
- Weight loss
- Itchy skin
What are the causes of jaundice?
Jaundice occurs when there is an excess of bilirubin. Bilirubin is a waste product of haemoglobin, which is the main content of red blood cells. This bilirubin is processed in the liver and transported through the bile duct into the small intestine, and eliminated in the faeces. Jaundice occurs when there is an increase in the rate of destruction of red blood cells, for example in certain liver diseases and in diseases where there is a blockage of the bile duct.
What are the different types of jaundice?
Types of jaundice are categorised by the area where the liver processes bilirubin that cannot be filtered into your digestive system for removal, and builds up to high levels in your blood. The types are:
- Pre-hepatic - this is before the liver
- Hepatic - this occurs in the liver
- Post-hepatic - this is after the liver
Pre-hepatic jaundice
This type of jaundice is caused by conditions that heighten your blood's rate of haemolysis. Haemolysis is the process where red blood cells are broken down, releasing haemoglobin and converting into bilirubin. The liver can only process so much bilirubin, so this means this excess overflows into bodily tissues.
There are several common causes of pre-hepatic jaundice, which are:
- Thalassemia - a condition that is genetic, which causes the body to create an irregular type of haemoglobin. This haemoglobin limits the number of healthy red blood cells in your blood stream.
- Sickle cell anaemia - where red blood cells become crescent-shaped rather than disc-shaped
- Spherocytosis - instead of disc-shaped red blood cells, the genetic condition causes them to be sphere-shaped
- Malaria - an infected mosquito bite that causes a blood infection
Symptoms of pre-hepatic jaundice include:
- Dark urine or pale stool
- Feeling itchy
- Abnormal weight loss
- Fever and cold sweats
- Abdominal pain
You are more at risk of developing pre-hepatic jaundice if you:
- Use drugs
- Have a family member with a blood disorder
- Travel to malaria-endemic regions
To make a diagnosis, there are different types of tests for pre-hepatic jaundice:
- A HIDA scan, which helps to find blockages or other problems in the liver, gallbladder, bile ducts alongside the small intestine
- MRI or ultrasound imaging tests, which examine your liver, gallbladder and bile ducts. These tests can rule out other forms of jaundice
- Blood tests, which measure bilirubin and other substances in the blood
- Urinalysis, which measures the amount of certain substances in your urine
Hepatic jaundice
When you have cirrhosis, which means your liver tissue is scarred, damaged or functioning incorrectly, it makes it less effective at filtering bilirubin from your blood.
As well as cirrhosis, hepatic jaundice can be caused by:
- Viral hepatitis, which is an inflammation of the liver caused by viruses from infected food, water or blood, alongside stool or sexual contact
- Liver cancer, where cancerous cells develop and multiply within liver tissues
- Alcoholic hepatitis, where liver tissues are scarred by the heavy, long-term drinking of alcohol
- Leptospirosis, a bacterial infection which can spread by infected animals, or infected urine or faeces.
- Primary biliary cirrhosis, which occurs when bile ducts are damaged and can't process bile. This causes it to build up in your liver and damage liver tissue.
The symptoms of hepatic jaundice can include:
- Vomiting
- Feeling sick
- Fever
- Darkening skin
- Muscle or joint pain
- Dark urine or pale stool
- Abdomen or leg swelling
- Abnormal weight loss
- Weakness
- Itchy skin
- Nose bleeding
- Loss of appetite
You are more at risk at developing hepatic jaundice if you:
- Have had previous liver infections
- Use medications that can cause liver damage, such as some heart medications and Acetaminophen
- Have drunk alcohol or used drugs for a long period of time
A diagnosis of hepatic jaundice can be made with the following tests:
- Endoscopy, which can be used to look at your liver and take a tissue sample, or biopsy, if analysis is necessary for cancer or other conditions.
- Imaging tests like MRIs or ultrasounds. They examine your liver for damage or presence of cancerous cells.
- Complete blood count (CBC) and antibody tests
- Liver function tests. Liver function tests measure bilirubin in the blood and levels of substances which indicate that your liver may not be processing bilirubin properly.
- Urinalysis, which measures substance levels in your urine related to your liver function.
Post-hepatic jaundice
Post-hepatic jaundice, also known as obstructive jaundice, is when bilirubin can't be drained properly into the bile ducts or digestive tract because of a blockage.
Common causes of obstructive jaundice are:
- Biliary atresia - This is a genetic condition where you have narrow or missing bile ducts.
- Bile duct cancer
- Pancreatitis
- Pancreatic cancer
- Gallstones
Post-hepatic symptoms include:
- Fever
- Abdominal swelling
- Weight loss that's abnormal
- Skin itching
- Diarrhoea
- Vomiting
- Dark urine or pale stool
- Feeling sick
Obstructive jaundice risk factors are:
- Having a family history of gallstones
- Smoking
- Drinking
- Pancreas inflammation or infection in the past
- Being overweight
- Having a diet that's high in fat and low in fibre
- Diabetes
Tests you can undertake to diagnose post-hepatic jaundice:
- Endoscopy
- Imaging tests
- Urinalysis
- Blood tests
How is jaundice treated?
In adults and young children, jaundice should be considered only as a symptom of a disease. Therefore, the treatment should not be for jaundice, but for the disease causing it. For example, if you have gallstones that are blocking your bile duct, which is one cause of jaundice, you might need medication or surgery.
How do I know if I have jaundice in my eye?
The whites of your eyes (sclera) can turn yellow when you have jaundice, as well as your skin. It's caused by the build up of too much bilirubin, a yellow substance that forms when red blood cells break down, in your blood, or due to the fact your liver can't get rid of it fast enough.
Causes of jaundice which may lead to yellowing of your eyes can be:
- Hepatitis
- Gallstones
- Drinking too much alcohol
- Medications such as steroids, Penicillin and Acetaminophen (taking too much), alongside birth control pills and Chlorpromazine, which is used to treat some mood disorders
- Liver infection
- Reaction to a blood transfusion
- Sickle cell anaemia
- Malaria
- Cirrhosis
- Non-alcoholic fatty liver disease
- Haemolytic anaemia
- Liver, pancreatic and gallbladder cancer
- Bile duct diseases such as biliary atresia, primary biliary cholangitis and primary sclerosing cholangitis
- Ulcerative colitis
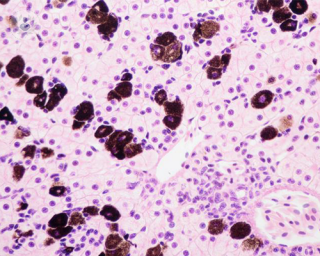
- Sarcoidosis, where collections of inflammatory cells called granulomas
- Amyloidosis, a rare disease where there's a build up of abnormal amyloid deposits in parts of the body such as the heart, brain, kidneys or spleen
- Pancreatitis
- Gilbert's syndrome, a genetic liver disorder which affects the body's ability to process bilirubin
Treatment for the cause of jaundice will help to get rid of yellow eyes.
Can jaundice occur in newborns?
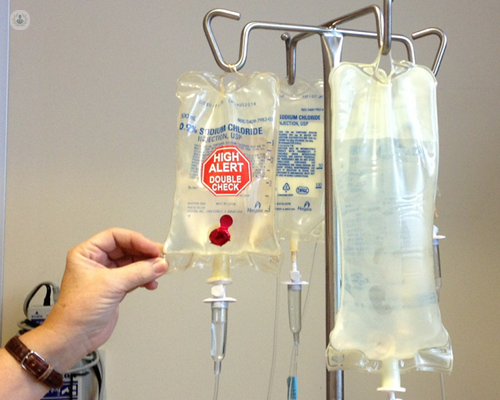
In newborns, jaundice can occur, but it usually goes away on its own. If the jaundice is mild, then parents should ensure the baby is feeding properly and is kept hydrated. If the jaundice is severe, then certain treatments may be indicated. Blood transfusion can be performed to clear the bilirubin from the blood, or light therapy (phototherapy) may be used in order to promote excretion of bilirubin.

Can jaundice be prevented?
There are some measures which can be taken to prevent jaundice such as:
- Avoiding excessive consumption of alcohol
- Receiving the hepatitis vaccine
- Avoiding certain medications (consult your doctor)
Which specialist treats jaundice?
There are a variety of specialists that treat jaundice. Gastroenterologists, hepatologists and general surgeons all treat conditions linked to jaundice.