Analysing bone strength – the DEXA scan
Written by:There are times in life when we will suffer broken bones and fractures, and it seems to happen to some people more frequently than others. This may be because some patients have a condition like osteoporosis, which leads fragile bones. Fortunately, doctors have the technology to analyse bone density. We talked to top rheumatologist and osteoporosis expert Dr Taher Mahmud, who explains all you need to know about the DEXA, or DXA scan.
What is a DEXA scan?
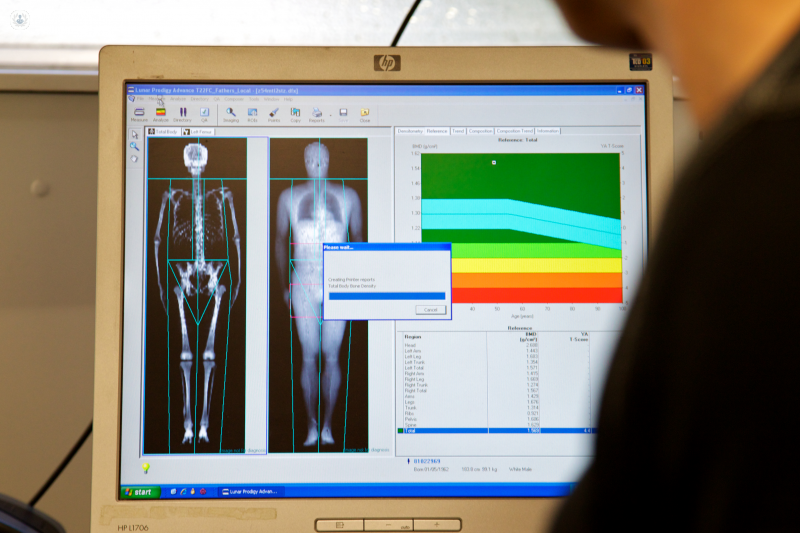
A DEXA (dual-energy X-ray absorptiometry; also abbreviated “DXA”) scan is a very low level X-ray used to quantify bone strength. The patient doesn’t feel anything – the procedure is painless and quite straight-forward to do. There are a number of different machines, which emit small x-rays. The operator sits in the same room as the patient and the machine. The radiation is minimal – it is the same level of radiation you might get sitting in plane or driving for 15 minutes; not much higher than normal background radiation.
What is a DEXA scan used for?
A DXA scan quantifies bone and can show the effects of osteoporosis (a condition in which the natural holes and spaces in bones are wider and so the bone becomes more fragile and more susceptible to breaks and fractures). A great number of things can lead to weaknesses in the bone – many different medical conditions such as coeliac, diabetes, and epilepsy; drugs, such as steroids and drugs used for prostate cancer; and general ageing. Patients may have issues with bones at any age.
With the help of a DXA scan, we can determine what the likelihood of a future fracture is; then we can implement multidisciplinary interventions. The good news is that with different interventions, bone strength can improve, and further DEXA scans can be performed to monitor its progress and appropriate adjustments can be made to the treatment if bone strength hasn’t improved.
In summary, DEXA is a well-established, safe, painless procedure, which takes about 20 minutes to do, and can give information on bones. Then we can do another DEXA in about a year’s time to see what the response to treatment is.
Very few people get a DEXA scan; more people should! 80% of people who have a fracture don’t get a DEXA scan, and go on to get more fractures. DEXA is helpful for arriving at a diagnosis.

When is a DEXA scan recommended?
We lose bone as we age. There are also a number of other situations, conditions, and risk factors that can lead to osteoporosis. Osteoporosis is a painless condition, and so it often goes unnoticed. It is worth doing a DEXA scan to assess the bones in the following situations:
- The patient has a fragility fracture (falling from a standing or sitting position).
- Older patients
- Perimenopausal women
- Certain medical conditions, e.g. coeliac, diabetes, thyroid issues, asthma, epilepsy, etc.
- The patient is taking certain drugs.
Can a DEXA scan show cancer?
It can show the effects of cancer, but it doesn’t diagnose it. It depends how the scan is done – DXA scans often take very general images. While it is not the main way of diagnosing cancer, osteoporosis and other problems with bone can be a consequence, which means that the results of a DXA scan could prompt the doctor to order more tests to check for the presence of cancer.
How long do you have to wait for DEXA scan results?
The results of a DEXA scan can usually be viewed almost immediately, but this may depend on the case. First, the scan is done; then the doctor needs to examine and interpret the results, before discussing them with the patient. This may be done on the same day.


