Osteoporosis: Causes and treatments explained
Written by:What is osteoporosis?
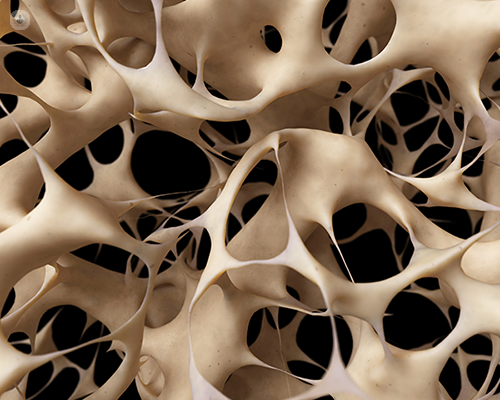
Osteoporosis is a common condition that can lead to pain, fractures and disability. The majority of patients are elderly women, but osteoporosis can also affect younger women and men. It is defined as a skeletal disorder characterised by compromised bone strength leading to an increased risk of fracture.
How is osteoporosis detected?
Bone strength reflects the integration of two main features: bone density and bone quality. Bone density is assessed using a DXA scan. Osteoporosis is defined in men and women over the age of 50 with a T-score of less than -2.5. However, bone density is just one aspect of osteoporosis. Osteoporosis is silent in most cases until the first fracture occurs. Fractures of the wrist, spine and hip cause pain, disability, loss of independence and patients often require long-term care.
In cases where osteoporosis is suspected, the patient should always see an endocrinologist
How many people are affected by osteoporosis?
More than one third of adult women and one in 12 men will suffer an osteoporotic fracture during their lifetime. Patients who have already suffered one osteoporotic fracture are at high risk of suffering subsequent fractures.
What are causes of osteoporosis?
Whenever there is a mismatch between bone formation and bone resorption the end result is a loss of bone density. Also, certain conditions increase bone turnover and increase the likelihood of fracture.
Factors which increase the likelihood of developing low bone density (BMD) are:
- Age
- Caucasian or Asian race
- Sedentary lifestyle
- Smoking
- Low body weight
- Family history of osteoporosis
- Excessive alcohol intake
- Excessive caffeine
- Prolonged calcium-deficient diet
- Long term use of certain medications: steroids, anti-oestrogens, anti-epileptic drugs etc.
- Oestrogen deficiency (surgical or natural menopause)
Other predisposing factors:
- Liver disease
- Malabsorption
- Inflammatory bowel disease (Crohn’s disease, ulcerative colitis)
- Thyroid disease
- Hypogonadism in men
- Primary hyperparathyroidism
- Rheumatoid arthritis
- Chronic renal failure
How can osteoporosis be treated?
Osteoporosis may be prevented by a healthy lifestyle including exercise and a balanced diet. Optimising calcium intake in diet and enabling normal vitamin D levels throughout your lifetime is essential for bone health.
Drug therapy is required for those at particularly high risk of having fractures. Treatment of individuals with established osteoporosis can prevent further fracture and improve the quality of life.
Currently available treatments for osteoporosis and fracture reduction are:
- Bisphosphonates Alendronic acid Risedronate Ibandronate (Bonviva) Pamidronate Zoledronic acid (Aclasta)
- Raloxifene
- Strontium Ranelate (Protelos)
- Teriparatide (Forsteo)
- Denosumab (Prolia)
Pros and cons of available treatments
All of the above treatment options except for teriparatide are antiresorptive drugs and they decrease the risk of fracture regardless of changes in BMD.
A practical problem with bisphosphonate therapy is that about 50% of patients discontinue treatment within one year. Common side effects are gastrointestinal symptoms like nausea, heartburn, oesophageal irritation, difficulty in swallowing. Patients also reported muscle and joint pains and with intravenous bisphosphonate there are often flu like symptoms (fever, muscle aches, headaches) within the first 24 - 48 hours after the injection. There are also growing concerns about long-term side effects, particularly osteonecrosis of the jaw and atypical hip fracture.
Read more: What can be done about a hip fracture?
Because of recognised problems and potentially serious side effects of bisphosphonate therapy clinicians are nowadays more cautious in making the decision to introduce this treatment. Significant benefit in preventing clinical fractures has only been documented in patients with previous vertebral or hip fracture or a hip BMD T-score of -2.5 or less.


