Bottoms up! Learn about anal fissures
Written by:It may be uncomfortable to speak about, but anal fissures are more common than people believe. What important information should people know about them? In this article, highly experienced consultant surgeon Mrs Katie Cross explains what anal fissures are, how they are caused and treated, and more.
What are the main causes of anal fissures?
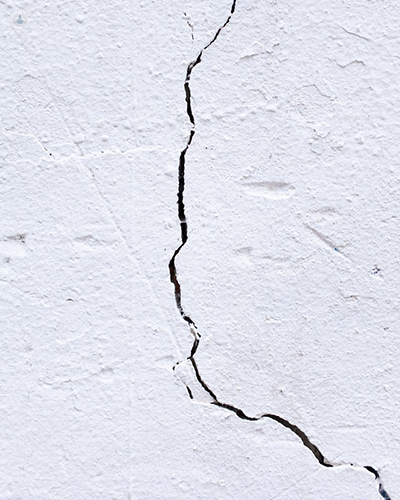
An anal fissure is a tear in the lining of the anal canal. Reduced blood flow at mostly the six o'clock position on your bottom, on your anus nearest to the backbone, rather than the front of your bottom causes the anal fissure to appear. Treating this reduced blood flow is how we try and heal anal fissures. It can be caused by, but is not limited to:
- Constipation
- Passage of a hard stool
- Diarrhoea
- Abrasion with cleaning yourself after passage of loose stool
- Inflammation in the bowel
- Stress related to pregnancy
- Haemorrhoids
- Poor toileting habits
Who is most affected by anal fissures?
Patients affected by anal fissures can be any age and by different causes. The majority of anal fissures are caused because of a high pressure in the anus which, again, reduces blood flow at this point.
Are they dangerous?
They are not dangerous in any way. However, they can cause significant discomfort; and that's why we treat them.
What are some lifestyle changes or home remedies that can help?
It's important to maintain a good toileting habit. Do not sit on the loo for longer than three minutes at any one time. Keep your stool soft and formed. If you develop an acute anal fissure and significant pain following defecation, then reduce the constipation with laxatives, maintain a very high fibre diet, drink lots of water, and keep your bottom clean and dry without using wet wipes. There is some evidence to suggest using salt baths.
If an anal fissure continues for more than six weeks, then it is called a chronic anal fissure. The GP will give you cream that will dilate the blood vessels at the back of your bottom, where the sore area is. This can be Rectogesic or Anoheal, and they may cause side effects including a headache. This headache is treated with paracetamol. You need to use the cream very sparingly—twice daily for two months every day—plus a laxative. This way, we can get sixty per cent of people healed without any further treatment.
If this treatment doesn't work, then I run a specialist clinic just for anal fissures which patients can attend. I will then offer them Botox in the outpatient setting, taking twenty seconds and improving a further ten per cent of patients. There are very small side effects to Botox, including bleeding, infection, temporary poor control, and, rarely, fistula formation.
How often is surgery carried out to treat this condition?
If the above treatments don't work, then we look at the cause of the fissure and treat that with surgery. This can either be by dividing the sphincter or by moving a flap of skin over the fissure to help it to heal. Alternatively, by treating the underlying problem.
If you think you may be experiencing anal fissures or would like more information, you can schedule a consultation on Mrs Cross’s Top Doctors profile.


