Piles (haemorrhoids)
What are haemorrhoids?
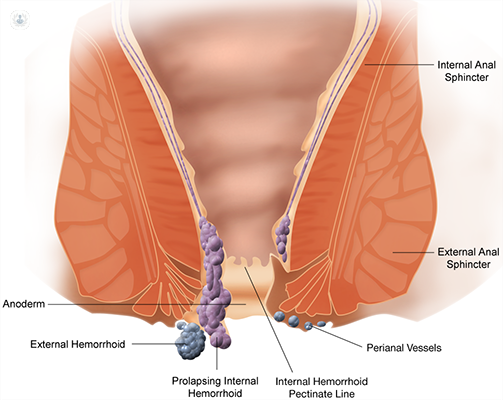
Haemorrhoids, commonly known as piles, are swollen veins in the anus or lower part of the rectum. They occur when the small veins that line the anal canal (the tube that connects the rectum and the anus) become engorged with more blood than usual. Together with overlying tissue, they form one or more swollen lumps (piles).
We are all born with haemorrhoids, but not all haemorrhoids will start causing symptoms. Symptomatic haemorrhoids are a very common ailment, and one in three adults in the UK will experience haemorrhoids at some point in their lives.
What are the different types of haemorrhoids?
Haemorrhoids may be either external (outside the anus) or internal (inside the anus). It's also possible to have both internal and external haemorrhoids at the same time.
External haemorrhoids usually generate protuberances in the ring of the anus on the outer side, which makes them easier to diagnose. They cause pain when sitting, in addition to traces of blood when defecating, and can prolapse (come out of the anus).
On the other hand, internal haemorrhoids start inside the anus, but they can hang down and prolapse too over time, causing bleeding in the stool and itching in the anal region.
Prolapsed haemorrhoids are graded into four different types, according to when they come out, and how far they come out of the anus:
- Grade I: Haemorrhoids bleed, but they remain in the anus
- Grade II: Haemorrhoids prolapse after passing a stool, but they go back inside on their own afterwards
- Grade III: Haemorrhoids prolapse after passing a stool but you need to physically push them back inside the anus
- Grade IV: Haemorrhoids are always prolapsed and can't be pushed back inside. If the blood inside them clots, they become thrombosed haemorrhoids, which bleed and are very painful
What are the symptoms of haemorrhoids?
Symptoms can vary between individuals and depend on the type of haemorrhoids that one has. Rectal bleeding, especially, should be consulted with a doctor, because this can be a sign for other pressing rectal and colon conditions - not necessarily haemorrhoids.
Internal haemorrhoids are usually asymptomatic, rarely causing pain, unless they prolapse out of the anus. If you have symptoms, this will include bleeding (usually bright red) from the rectum.
The main symptoms of external haemorrhoids are:
- Bleeding (bright red) from the rectum when passing stool, or present in the faeces
- Anal itching or soreness
- Feeling of an 'incomplete' evacuation
- Pain or discomfort in the anus, especially when sitting
- Swelling near the anus
- Pain when passing stool
- Feeling one or more hard and tender lumps in, or near, the anus
- Flow of mucus after passing stool
What causes haemorrhoids?
The exact cause of haemorrhoids depends on the person. Studies have shown that their development is connected to an increased pressure (straining) in the anus, which interferes with the blood flow and causes the veins to stretch and bulge. This can be caused by:
- Effort during bowel movements
- Constipation or long-lasting diarrhoea
- Sitting (on the toilet) for extended periods of time
- Pregnancy or childbirth
- Obesity
- Regular heavy lifting
Ageing also increases your risk of haemorrhoids. This is because the supportive tissue that holds the haemorrhoids in place weakens and stretches with age, making it more likely for the haemorrhoids to engorge and prolapse.
Can they be prevented?
To prevent haemorrhoids, it is necessary to avoid constipation and avoid any activity that puts increased pressure on the anus. For this reason, it is important to:
- Drink plenty of hydrating liquids - water in particular - and cut down your alcohol and caffeine intake
- Eat a diet rich in fibre
- Use stool softeners to prevent straining if you are constipated
- Keep your anus clean and dry
- Exercise frequently
- Not ignore the need to evacuate, and avoid spending more time than needed when you are in the toilet
- Avoid medication that contains codeine, as it can cause constipation
How are haemorrhoids treated?
In the case of external haemorrhoids, the treatment consists of applying creams or suppositories, and warm water in the affected area. In cases of severe pain, you can take over the counter painkillers.
For internal haemorrhoids, minimally invasive procedures, like rubber band ligation, or surgical intervention may be necessary to remove them.
What happens if haemorrhoids are left untreated?
Most, mild, haemorrhoids will go away on their own within a few days, or weeks. You can reduce the irritation and discomfort with the help of at-home treatments.
Prolapsed haemorrhoids tend to worsen with time. Although rare, complications can happen if haemorrhoids are left untreated, such as:
- Trapped haemorrhoids outside the anus
- Painful blood clots
- Irritated skin tags
- Lower amount of red blood cells, leading to anaemia
- Loss of blood supply, in the case of strangulated haemorrhoids
















