What really happens when you have macular degeneration?
Written by:Macular degeneration is the commonest cause of severe central visual loss in the Western world. The risk of developing it is around 1 in 3 for those over 75, the risk increases exponentially with age, and it is 30% commoner in females. If you have a mother or father, brother or sister who has the condition, your risk of developing it is increased fivefold. People find the diagnosis worrying; they take it as an indication of ageing and mortality, and they fear becoming dependent on others. After all, much of what gives pleasure is visual. Mr Jonathan Dowler, a leading ophthalmologist and macular degeneration expert, explains what really happens with this diagnosis.
What is the macula?
It is part of the receptive film, the retina, which lines the back of your eye. If somebody walks into the room, you see the movement out of the corner of your eye, and you move your head and eyes to look at them. What you are doing is to line up that part of your retina responsible for detailed vision, the macula. You move your eyes when reading a book to line your macula up with the words.
When you get macular degeneration, it is this area of the retina that is damaged. Surprisingly, the macula accounts only for a very small amount of the retina, and the rest of it is not damaged by macular degeneration and continues to work as before.
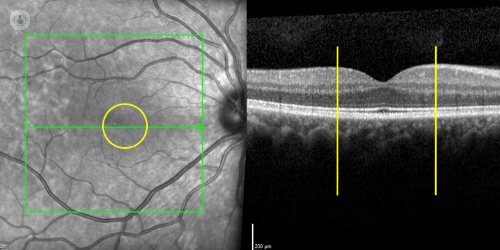
The macula is shown as the yellow circle on the image of the retina on the left, and between the yellow lines in the cross sectional view on the right.
How does the macula work?
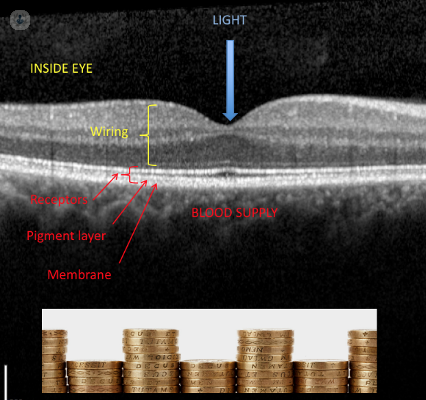
Below is a cross-sectional image of the retina at the macula. Light travels towards the retina in the direction of the arrow. Light is received by receptor cells which can be seen as the fine parallel lines at the bottom of the image. These cells convert the light energy into electrical impulses, which are picked up by other cells, integrated, and passed via the optic nerve, to the brain.
What happens in macular degeneration?
Most people think of macular degeneration as being either wet or dry. However, most people with macular degeneration have neither; they have early macular degeneration, which is neither wet nor dry.
Early macular degeneration:
Early macular degeneration does not cause significant visual problems, it just has the potential to develop into wet or dry macular degeneration, which do cause visual problems. The risk of this happening can be quantified, and reduced with vitamins and antioxidants. The elements of the receptor cells are like a stack of coins which are replenished from above, and shed from below into the bloodstream. To get into the bloodstream they have to pass through a membrane. In macular degeneration, this process is defective, and deposits accumulate underneath the retina. This separates the receptor cells from their blood supply. In early macular degeneration, these deposits can be seen when examining the eye; shown as arrows below.

Looking at the retina, it is possible to predict the likelihood that the eyes go on to develop wet or dry macular degeneration over the next 5 years. These vary from 3 to 50% . This risk can be reduced by 25% by taking a particular combination of vitamins and antioxidants; PreserVision AREDS 2 was the formulation used in the most recent study. This is available over-the-counter and online.
Dry macular degeneration:
Dry macular degeneration moves slowly and eventually stops. You will never go blind, your brain will adapt to the problem, and you should be able to lead an independent existence. Treatments are likely to become available. In dry macular degeneration, retinal tissue fades away, because is separated by the deposits from the bloodstream. This is a very slow process. Bare patches appear; see arrows below: aerial view to the left, cross section to right.

As the disease progresses, central vision very gradually gets worse, but typically stabilises after some time. It is not possible to halt dry macular degeneration at present, though this is a field of intense research. However, as the disease develops, the brain learns to use other parts of the retina which still work to see with, so function is often surprisingly good. There is also a staggering range of devices to help, particularly electronic ones.
Wet macular degeneration:
Wet macular degeneration moves quickly, but if identified and treated promptly, and checked frequently, can have an excellent long-term outcome. In wet macular degeneration, the retina which is deprived of its blood supply produces a chemical. This chemical makes blood vessels grow into the retina. They leak, bleed, and scar and damage vision. This can occur quite rapidly.

People who develop wet macular degeneration commonly notice that straight lines have become bent, or that a blank patch has appeared in the vision. If this happens, it is an emergency, and needs to be looked at by a retinal specialist straight away. Injections into the eye can stabilise vision in 90% of cases, and about 1/3 of cases are substantially improved.
If you are concerned about macular degeneration, make an appointment with a specialist.


