What is age-related macular degeneration (AMD)?
Written by:Did you know that age-related macular degeneration (AMD) is the biggest cause of sight impairment in the UK? But what is this eye condition? What does it do to the eyes, and how does it impair vision? Internationally recognised ophthalmologist Mr Praveen Patel provides the answers you need about macular degeneration.

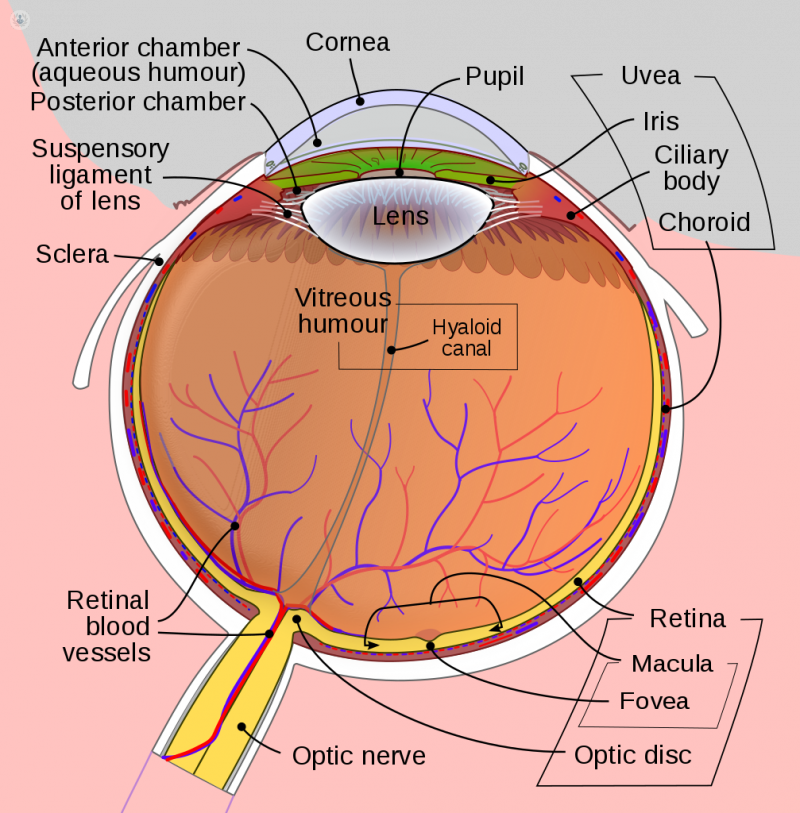
Know your anatomy
Before we get started on the disease, here’s a refresher on the part of the eye affected:
- The retina – the layer of light-detecting cells at the back of the eye. The retina is essential for vision, acting like the film in a camera. The light that enters the eye triggers chemical reactions in its cells, which send impulses to the brain, giving it the information it needs to form an image.
- Rods – A type of light-detecting (photoreceptor) cell in the retina. Rods work well in dim light, and are largely responsible for our night vision. They do not contribute much to colour vision, which is why colours are less clear in the dark.
- Cones – The other type of photoreceptor cell. Unlike rods, cones work better in brightly-lit environments, and function poorly in the dark. They provide colour vision, and respond to light faster than rods, giving us the ability to see in finer detail. Human beings have 3 types of cones, each giving a different range of colours.
- The macula – a small, yellow oval part of the retina, located near the centre. Due to the high concentration of cone cells, it is responsible for high-definition central colour vision.
What happens to our vision without the spectacular macula?
As you may have guessed, macular degeneration involves a loss of function in the macula. There are two types of AMD:
- Dry AMD – the most common. Little pockets of extracellular material called “drusen” commonly occur beneath the retina in people over 50 years old, which is associated with subtle problems with vision such as poor vision at dawn and dusk when lighting is poor. As dry AMD worsens, vision deteriorates over months or years.
- Wet AMD – less common, but more serious, with rapid onset. Sometimes called neovascular AMD, the macular photoreceptor cells are damaged by abnormal blood vessels which typically grow from underneath the macula into the photoreceptor layer. Vision can deteriorate within days. Thankfully we now have effective treatments for wet AMD which are given as eye injections.
As both forms of AMD affect the cone cells of the macula, central colour vision becomes impaired – colours appear faded; fine detail decreases, with vision becoming more and more blurred; and it can become difficult to read or distinguish faces as the disease worsens.
AMD: Fast facts
- AMD currently affects 600,000 people in the UK (the country’s leading cause of vision loss).
- This is predicted to rise to over 700,000 by 2020.
- AMD is more common in men than women, and is more common in white and Chinese patients than in other ethnicities.
- You are more likely to get AMD the older you get. 1 in 10 people over the age of 65 have some form of this eye condition.
- Age-related macular degeneration affects our ability to carry out everyday tasks such as reading, recognise faces and driving.
- Age-related macular degeneration is unlikely to cause total blindness, as it does not affect peripheral vision.
- While there is no cure, there are treatments to manage AMD by slowing the progression of the condition and/or using glasses or lenses to see as well as possible.
If you are experiencing any of the visual symptoms mentioned in this article, you should consult your doctor or a specialist in the assessment and treatment of retinal disease.


