Blurred lines? All about macular degeneration
Written by:Macular degeneration (AMD), also known as age-related macular degeneration, can lead to blurriness or no vision in the central field of vision. Despite AMD being a natural occurrence, there are ways to slow down and even reverse any vision loss that people may have.
Here to offer a detailed insight to the condition, particularly when it comes to delaying AMD is highly experienced consultant ophthalmic surgeon Mr Allaaeldin Abumattar.

What is macular degeneration?
Age-related macular degeneration (AMD) is a condition that naturally occurs with ageing. It tends to result in gradual deterioration of central vision due to the irreversible wear and tear of sensitive cells at the back of the eye (photoreceptors), characterised by slow deterioration of central vision, which may - in some cases - lead to irreversible central vision loss. The central vision is the most used part of our eyes. It picks out fine details, colours and shapes of objects to create a crisp, clear picture. It allows us to read, drive, dial the telephone, recognise faces and see objects; to perform our daily tasks and routines.
What is the main cause of macular degeneration?
Causes of AMD are not fully understood, but increasing age, genes, weight, diet, and some lifestyle factors are known to increase the chances of developing it.
The sensitive cells at the back of the eye (photoreceptors) sit atop a layer of cells called retinal pigment epithelial cells (RPE). The RPE layer does a very important job in our eyes. It transports oxygen and essential nutrients to photoreceptors and recycles their waste products. As we age, the RPE layer loses its effective recycling leading to the accumulation of ‘waste’ in the RPE layer called drusen. Drusen, genetic and environmental factors ultimately damage our aging photoreceptors.
Who is most at risk of macular degeneration?
A person’s risk of developing AMD increases with age. In the UK, AMD affects over 600,000 people where about one in 20 people aged over 65, and about one in eight people aged over 80 have AMD severe enough to cause serious visual loss.
Having a first-degree relative diagnosed with AMD increases the relative risk of developing it. It’s important here to emphasise that it’s not only genetic factors that play a role in AMD development. Drusen (sensitive cells waste), genetic and environmental factors all contribute. Genetics alone are not definitive for the occurrence or progression of the disease. Patients that have genotypes that are known to be high-risk may not develop AMD.
Can macular degeneration be prevented? If so, how?
The good news is that our knowledge and recent advances in AMD treatment are helping to slow down and prevent further worsening - and sometimes reverse - the vision loss caused by AMD. Ways to prevent or slow the disease are:
-
Stopping smoking
It’s been consistently shown in research how smoking increases the risk of developing AMD. It’s been found that current smokers are up to four times more likely to have AMD in comparison to people who’ve never smoked.
Smokers are more likely to develop AMD up to 10 years earlier in comparison to those who have never smoked.
AMD in smokers is likely to progress faster and be less responsive to treatment.
The risk of AMD is also likely to increase if a person is around second-hand smoke.
Stop smoking services can help you to quit. You’re up to four-times more likely to quit successfully with the help of these services.
-
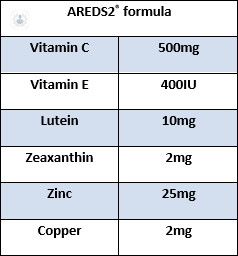
Dietary supplements vs Age Related Eye Disease Study 2® (AREDS2®)
The damage that oxidant substances can cause, can be negated by certain nutrients that protect the body. Antioxidants reduce the harmful effect of oxidants. Examples of antioxidants are vitamins A, C and E. Lutein and zeaxanthin are pigments on our eyes that act as a natural sunblock to protect our central vision. Our body cannot make them. They must be consumed in food. Several studies suggest that at least 10mg of lutein a day has the most beneficial effect on our central vision, and diet alone cannot provide the sufficient levels of vitamins and minerals required for AMD risk reduction. The average western diet contains no more than 3mg of lutein and zeaxanthin a day.
Kale is the best source of lutein, even when raw. Lutein and zeaxanthin are found in eggs, and they may be absorbed more easily by the body because they’re eaten with the fat that’s contained in the egg. Orange and yellow fruits and vegetables such as sweetcorn and orange peppers contain zeaxanthin, and many of them also contain vitamins C and E.
Milligrams (mg) of lutein per 100g fresh vegetables: 11.4 mg in kale, 8.5 mg in red pepper, 7.9 mg in spinach, 4.7 mg in lettuce, 3.6 mg in leek, 3.3 mg in broccoli, 1.7 mg in peas.
AREDS2® dietary supplements will not prevent or cure AMD. They may just delay the progression of AMD to help you keep your vision longer. AREDS2®can lower the risk of getting late AMD in the other eye.
AREDS2® can reduce your risk of developing advanced AMD by about 25 per cent after 5 years of using the formula.
-
Know your family history
Those who have a first-degree relative that is, or has been, affected by AMD, have a significant risk of developing it. These people should look out potential symptoms, which include difficulty recognising faces, struggling to adapt to low light and seeing straight lines that appear wavy.
If macular degeneration is treated, can it reoccur?
AMD has no cure yet. However; treatment options available can control the disease successfully in most of patients. It is essential to keep regular follow ups. Studies show that, on average, patients need between six to eight eye injections a year to control wet macular degeneration recurrence. Some patients may need fewer, some patients more, but long-term, sustained AMD treatment is important to treat recurrence of the disease.
Since wet AMD involves scarring that cannot be reversed, early detection of wet AMD is critical. Patients typically have more satisfactory results with anti-VEGF treatment when AMD is caught early, before significant scarring has occurred. One third of treated patients might get some of their lost vision back after treatment. Nine out of 10 patients have a chance of treatment being successful in preventing central vision loss from worsening.
Most people with macular degeneration have the more common form, dry AMD, in one or both eyes. In one out of 10 people, dry AMD progresses to wet AMD.
If you’re looking for expert treatment for AMD or other ophthalmic issues, arrange an appointment with Mr Abumattar via his Top Doctors profile.


