Hysteroscopy: pain relief, postoperative bleeding and periods
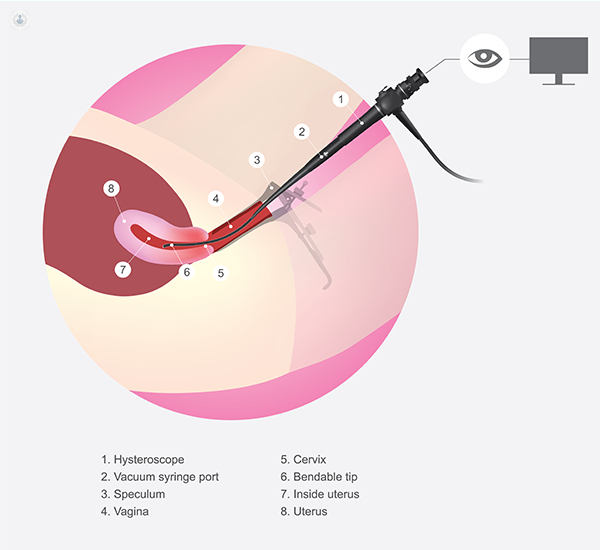
Written by:A hysteroscopy is a diagnostic and operative test that’s performed using endoscopy equipment (a long, flexible tube with a camera at the end) to directly visualise the endometrial cavity (the inside of the uterus).

Why we use hysteroscopy
We use the hysteroscopy procedure to look inside the uterus (also referred to as the womb) with a camera. It can be used for diagnostic and operative purposes.
The objective is generally to identify the cause of any menstrual irregularities. This could be:
- Menstrual disorders in women of any age before menopause (e.g. heavy bleeding, bleeding between periods)
- Fertility concerns
- Bleeding after menopause
- Abnormal discharge
- Retained products of pregnancy tissue
- Uterine fibroids
- Uterine polyps
The timing of a hysteroscopy
You can have a hysteroscopy at any point in your cycle, as long as you’re not bleeding. We don’t advise you to come in while bleeding because the blood mixes with water (the water we insert to distend the cavity) and clouds the picture we see through the endoscope.
Pain relief during hysteroscopy
Patients always ask me about pain relief. Hysteroscopy can be done either:
- While the patient is awake in an outpatient clinic with pain relief, local anaesthetic and sedation
- In theatre with a general anaesthetic
Which pain relief is best?
The option of pain relief is purely dependant on patient choice, previous experiences and background history. I always emphasise the importance of a detailed discussion between the gynaecologist and the patient about pain relief before agreeing on the location of the procedure. Under no circumstances should anyone be forced into either option. It should be an informed decision after a conversation between you and your doctor.
With the advances in medicine and equipment, outpatient hysteroscopy is more accessible and widely promoted in ambulatory gynaecology. If you have a hysteroscopy in an outpatient clinic, you might choose to have:
- Local anaesthetic (you remain conscious but the pain is reduced in the target area)
- Painkillers (that you can take during and after the procedure)
- Both
If you have local anaesthetic and/or painkillers, you don’t need anyone to come with you to the clinic, or take you home. If you choose to have a general anaesthetic in theatre, you’ll be unconscious during the procedure and someone will need to help you travel home.
Know your pain threshold
The procedure can be painful at times. Therefore, it’s important to identify your personal limitations and assess the need for anaesthetic. Some women find hysteroscopy really painful if it is done in an outpatient setting. If you do find it painful, it’s very important to stop the process and reassess with your doctor so that they can provide more pain relief.
Bleeding after a hysteroscopy
Bleeding after a hysteroscopy can be normal. This is because we use water to distend the cavity of the uterus so that we can visualise it and see clearly. So, as a result, the lining of the cervix and womb can be irritated during the insertion of the endoscope (the rod-like structure with a camera at the end), which causes bleeding.
Most of the time, what comes out is mainly water-based but mixed with some blood. It’s unlikely that the bleeding will be similar to a period.
When to contact the doctor about bleeding
As a fail-safe, we (doctors) tell women that if their bleeding is unusual for them after a hysteroscopy, seek medical attention.
If you’re bleeding heavily where you need a pad, I recommend contacting the unit or surgeon immediately on the same day. Then we can assess the underlying reason and determine if the bleeding is related to the procedure (the irritation of the uterus) or a complication of the procedure (e.g. like an accidental hole in the uterus lining. However, complications are very rare.
The first period after a hysteroscopy
The first period after a hysteroscopy should be the same as periods before the procedure unless we performed a treatment during the procedure (e.g. the removal of an endometrial polyp or fibroid). If a woman had heavy periods before the procedure and we remove the polyp or fibroid, they can expect the periods to get much lighter.
Signs of hysteroscopy complications
Overall, we know that hysteroscopy complications are very rare in general. The procedure is one of the most straightforward processes that we perform in gynaecology.
Infection
Just like any procedure, there is a small risk of introducing an infection using tools inside the body. We take several measures to prevent this, but contact your gynaecology unit if you experience one or more of the following after a hysteroscopy:
- Offensive smelling discharge
- Discharge of an unusual colour
- A hot and cold fever
Then, we can take swabs to check for infection and treat it immediately.
Perforation
Perforation during hysteroscopy is extremely rare. During the dilatation of the cervix, it’s possible to make a hole in the uterus, which could harm the organs outside it. However, this would be recognised, assessed and fixed immediately.
In these cases, we assess the depth of the injury and check if a repair is required. We offer either:
- Laparoscopy (also known as minimally invasive surgery and keyhole surgery)
- Open surgery (a more invasive option in which we cut through the abdomen to have a look from above).
But remember, perforation is an extremely rare complication.
Following a hysteroscopy, you should be given a post-procedure leaflet with the recovery timeline and contact details of who to speak to if things don’t seem right.
Dr Marina Fernando is dedicated to providing personalised and safe obstetric and gynaecological care – visit her profile to discover how she can help you.


