Hysteroscopy
Mr Andrew (Ted) Baxter - Obstetrics & gynaecology
Created on: 11-13-2012
Updated on: 10-03-2023
Edited by: Conor Lynch
What is a hysteroscopy?
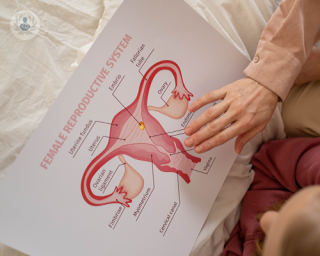
A hysteroscopy is a clinical procedure that allows the specialist to view the cervix, the inside of the uterus, and the openings of the fallopian tubes to study the functions and shape of the endometrium. There are two types of hysteroscopy:
- Ambulatory, or in-clinic, to diagnose and treat uterine pathologies without surgical intervention.
- Diagnostic: where a hysteroscope (a lighted tube) is inserted into the cervix to view the inside of the uterus. If samples are also taken, or if endometrial formations are resected, or surgery is performed, it is known as a surgical hysteroscopy.

Why is a hysteroscopy performed?
A hysteroscopy is performed in the following cases:
- irregular menstruation or metrorrhagia
- to perform sterility or infertility studies, recurrent miscarriages
- to diagnose changes in the shape of the inside of the uterus, such as polyps, fibroids or hyperplasia, as well as to detect foreign bodies or traces of placenta
- to study and control malformations of the uterus
- to block the fallopian tubes to prevent pregnancy
- to remove an IUD
- to perform a biopsy
How is a hysteroscopy performed?
The patient lies down and is placed in the gynaecological examination position. An instrument is inserted into the vagina to widen it (a speculum), and the vagina and the inside of the uterus is cleaned using an iodine solution. The cervix is then held in place with a clamp. The specialist adapts the hysteroscope to the size of the vaginal canal and slowly inserts it.
The hysteroscope is a lighted tube connected to a video camera and a screen. In some cases, gas or fluid may be introduced into the uterus to expand it so that the inside of the uterine cavity can be seen better. Local anaesthetic may be applied to the cervix, if necessary. To remove abnormal growths or tissue for testing, tools may be placed inside the hysteroscope.
How should I prepare for my hysteroscopy?
Prior to a hysteroscopy, the specialist may prescribe medication that opens the cervix, which should be taken eight to 12 hours before the procedure. It's important that you tell your doctor about any medication you are taking, including:
- vitamins;
- herbs, or dietary supplements;
- and also if you have any health problems,
- if you are pregnant, or;
- if you smoke.
On the day of the surgical hysteroscopy, you should not eat or drink anything in the hours prior to the procedure, and the indicated medication should be taken only with a small amount of water.
What does post-surgery recovery entail?
You can return home on the day of the procedure, as hospital admission is necessary only in a few cases.
You will be able to return to normal daily life within two days of the procedure, but it is very important to abstain from sex until the specialist tells you that you are well enough to do so. You might experience menstrual-like cramps and some slight vaginal bleeding for a couple of days afterwards. For cramps, ask your specialist if you can take pain medicine. During the following few weeks, you may notice some watery discharge.

Which specialist performs hysteroscopies?
Obstetricians and gynaecologists are the specialists who typically perform hysteroscopies.
Is a hysteroscopy painful?
It must be said that this varies from woman to woman. Some women feel no or only mild pain during a hysteroscopy, whilst others can experience intense and severe pain. If the patient is worried about the pain they might experience during the procedure, they should speak to the doctor or nurse before having the procedure with regards to what to expect and to also ask them about pain relief options.
What are the main risks involved?
A hysteroscopy is, generally speaking, a very safe procedure for patients. Having said that though, like any procedure, there is a small risk of complications. It is important to note here that the risk of potential complications is higher for women who are undergoing other specific medical treatment during a hysteroscopy.
Some of the main risks associated with a hysteroscopy include the following:
- infection of the womb
- feeling faint or lightheaded
- damage to the cervix
- damage to the womb
- excessive bleeding either during or after surgery
- smelly vaginal discharge
What are the main alternatives to a hysteroscopy?
There are two main alternatives to a hysteroscopy if the patient does not feel comfortable undergoing a hysteroscopy or if their doctor deems them not to be a suitable candidate for it. These are:
- Pelvic ultrasound.
- Endometrial biopsy
Patients should note that a hysteroscopy is more effective when compared to these two techniques.